Overview
Interoperability in healthcare is essential for effective communication and data sharing among diverse information systems, devices, and applications. This capability is crucial for enhancing patient care and operational efficiency. However, achieving interoperability presents significant challenges, including:
- A lack of standardization
- The reliance on outdated legacy systems
Furthermore, the integration of advanced technologies such as FHIR and hybrid integration platforms is vital for facilitating seamless data exchange. As a result, these innovations can significantly improve healthcare outcomes. Are you ready to embrace these technologies and overcome the barriers to interoperability?
Introduction
In the rapidly evolving landscape of healthcare, interoperability emerges as a critical pillar for enhancing patient care and operational efficiency. Defined as the ability of various information systems and applications to communicate and exchange data seamlessly, interoperability transcends mere technical requirement; it is a necessity for delivering high-quality healthcare.
As the industry shifts towards a more connected ecosystem, understanding the nuances of interoperability—from foundational principles to advanced semantic frameworks—becomes essential. Despite its clear benefits, many healthcare providers remain hesitant, often unaware of the transformative potential that effective data exchange can unlock.
This article delves into the multifaceted dimensions of interoperability, exploring its significance, the challenges faced by healthcare organizations, and the innovative solutions paving the way for a more integrated future.
Understanding Interoperability in Healthcare
Interoperability in healthcare refers to the capability of diverse information systems, devices, and applications to communicate, exchange, and utilize information effectively. This capability is essential for medical providers, enabling them to access and share individual information effortlessly, thereby enhancing care coordination and improving patient outcomes. Interoperability encompasses various levels, from basic data exchange to complex integrations that facilitate comprehensive data utilization across multiple platforms.
As medical systems evolve, the demand for system compatibility intensifies, particularly in 2025, where the focus is on enhancing efficiency and ensuring patient safety. A significant challenge remains, as some healthcare providers do not fully recognize the benefits of system integration. For instance, a representative noted that while immediate access to lab results is achievable, certain providers are comfortable with existing delays, revealing a gap in understanding the critical nature of system compatibility.
This mindset can obstruct broader adoption and integration efforts, as not all stakeholders perceive its immediate advantages. Recent statistics reveal that out of 38 organizations invited to participate in interviews about compatibility, only 20 engaged, highlighting ongoing challenges in fostering a unified approach to information exchange. Moreover, medical leaders stress the importance of effective information exchange, with one stating, “It’s one of those things where now you’ve got to subscribe to it [e.g., a regional HIE], and it’s another place [e.g., application] for you to go to look for more information [e.g., patient clinical records]…There’s too many places for information to land and get sent. People just stop looking.”
This underscores the necessity for efficient solutions that uphold the definition of interoperability in healthcare, facilitating access to critical information. Avato’s hybrid integration platform is designed to address these challenges by accelerating secure system integration for medical providers. By unlocking isolated assets and enabling seamless information connectivity, Avato improves operational visibility and issue resolution, ensuring that healthcare organizations can adapt to evolving demands. Successful instances of system integration demonstrate its potential to transform healthcare.
By enabling real-time data exchange and enhancing communication among providers, seamless integration can significantly elevate health outcomes. However, some healthcare providers remain skeptical about the benefits of system integration for patient care. A representative remarked that although immediate access to lab results is possible, some providers are content with current delays, indicating a gap in recognizing the significance of system compatibility.
This viewpoint presents a challenge in advancing the interoperability in healthcare definition, as not all providers acknowledge its immediate benefits, potentially hindering broader adoption and integration efforts. As the medical landscape continues to evolve, the importance of a reliable and future-proof technology stack becomes crucial. Avato’s commitment to architecting the necessary technology foundation for rich, connected customer experiences positions it as a leader in simplifying complex integrations and delivering cost-effective solutions. This enables organizations to maintain a competitive edge in providing quality care.

Types of Interoperability: Foundational, Structural, and Semantic
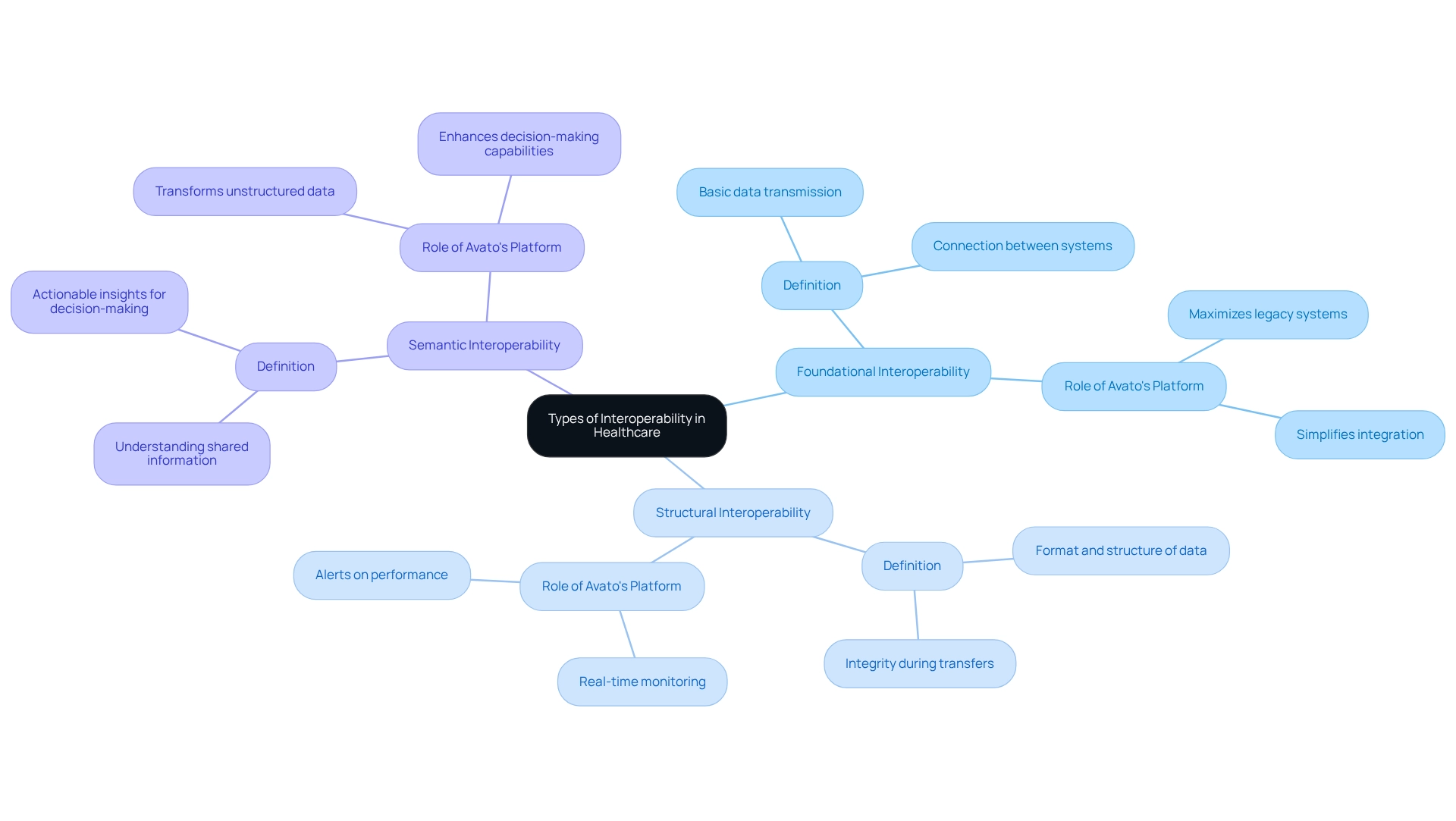
The interoperability in healthcare definition underscores its critical role in medical services, facilitating seamless information exchange. This concept can be classified into three main types: foundational, structural, and semantic.
Larry Ellison, founder and CTO of Oracle, astutely questioned the disparity between financial and medical information systems. He emphasized the urgent need for a global medical database that ensures vital patient information is readily accessible during emergencies. This observation highlights the persistent challenges and opportunities within the interoperability in healthcare definition.
- Foundational Interoperability serves as the essential base for information exchange, enabling one system to transmit data to another. This fundamental level is crucial for establishing connections between disparate systems, allowing for the initial sharing of information. Avato’s Hybrid Integration Platform excels in this domain, maximizing and extending the value of legacy systems, thereby simplifying the integration process.
- Structural Interoperability builds upon this foundation by defining the format and structure of the exchanged information. This ensures that the receiving system can accurately interpret the data, preserving integrity during transfers. Without structural compatibility, the risk of miscommunication and information loss significantly increases. Avato’s platform provides real-time monitoring and alerts on system performance, ensuring that structural integrity is maintained throughout the information exchange process.
- Semantic Interoperability represents the pinnacle of system compatibility, where both systems not only share information but also understand its significance. This level is crucial for generating actionable insights, as it enhances clinical decision-making by ensuring that the data is both relevant and comprehensible. Avato’s commitment to developing technological frameworks supports this degree of compatibility, enabling organizations to transform unstructured data into structured requirements models that enhance decision-making capabilities.
Current trends indicate a growing emphasis on interoperability in healthcare definition, particularly as medical systems strive to create a cohesive global health network. Health information exchanges (HIEs) and qualified health information networks (QHINs) are leading this movement, aiming to improve patient care and public health research.
Statistics reveal that a significant portion of studies—approximately 11.9%—utilize an ontology-based approach to enhance compatibility, underscoring the importance of organized information in medical fields. Moreover, expert insights highlight the necessity of developing a learning health system that aligns with the interoperability in healthcare definition, reduces costs, enhances population health, and drives continuous innovation. Avato’s platform notably decreases costs associated with complex integrations, making it an invaluable asset in this endeavor.
A notable case study titled ‘Accelerating Research and Innovation in Healthcare’ illustrates how system compatibility fosters advancements in AI-driven diagnostics and personalized medicine. By organizing medical data for machine readability, organizations can leverage predictive analytics to optimize resource allocation and public health planning. The findings from this case study demonstrate that enhanced collaboration can lead to more effective medical service delivery and improved outcomes for individuals.
As we approach 2025, the focus on foundational, structural, and semantic interoperability will continue to advance, with industry leaders advocating for systems that can adapt to evolving demands. Avato’s commitment to simplifying disparate systems and enhancing business value positions it as a pivotal player in this ongoing transformation.
The Importance of Interoperability in Enhancing Patient Care
The definition of interoperability in healthcare is vital for enhancing healthcare delivery by enabling providers to swiftly and effectively access comprehensive individual information. When systems embody the principles of interoperability in healthcare, clinicians can significantly reduce redundant tests, minimize medical errors, and enhance care coordination. For example, statistics reveal that 74% of hospitals have successfully integrated information into their Electronic Health Records (EHRs), leading to fewer adverse events and improved patient satisfaction scores.
Moreover, the definition of interoperability in healthcare underscores the necessity of efficient integration for timely access to medical records, which is crucial for informed clinical decision-making, particularly in emergency scenarios. As Loyd Bittle, CEO of Innovar Healthcare, emphasizes, understanding interoperability in healthcare is essential for organizations striving to deliver quality patient care and operate effectively. A notable case study is the Department of Veterans Affairs (VA), which faces significant challenges in achieving seamless integration as it transitions from its long-standing EHR system, VistA, to Cerner’s MHS Genesis.
This initiative, projected to exceed $4 billion and take up to 10 years, highlights the complexities involved in modernizing medical systems. The integration of compatible systems not only streamlines the medical experience for both providers and patients but also substantially enhances patient outcomes, demonstrating the transformative impact of interoperability in healthcare within contemporary medical practice. Furthermore, as Gustavo Estrada points out, Avato simplifies intricate integration projects, delivering results within established time frames and budget constraints.
Avato offers a dedicated hybrid integration platform that supports 12 levels of interface maturity, expediting secure system integration across banking, medical, and government sectors. This platform effectively balances the speed of integration with the complexity required to protect technology stacks, positioning Avato as a crucial partner for organizations seeking to achieve seamless operations. Originating from a team of enterprise architects committed to addressing complex integration challenges, Avato embodies a dedication to delivering connected customer experiences.
Challenges to Achieving Interoperability in Healthcare Systems
Achieving interoperability in healthcare within medical systems is essential yet fraught with significant challenges. Key obstacles include:
- Lack of Standardization: The absence of uniform data formats and terminologies across different systems complicates seamless information exchange. This inconsistency obstructs effective communication among medical practitioners, ultimately affecting care for individuals.
- Legacy Systems: A staggering 70% of healthcare organizations in 2025 continue to rely on outdated technology that lacks interoperability capabilities. These legacy systems create silos of information, making it difficult to access and share essential medical information efficiently. Avato’s hybrid integration platform addresses this issue by bridging the gap between legacy systems and modern expectations, enabling organizations to unlock isolated assets and enhance business value.
- Information Privacy Concerns: Safeguarding individual information while allowing for information sharing presents a considerable challenge. The possibility of breaches in information not only threatens patient confidence but can also result in serious legal and financial consequences for healthcare entities. Avato’s commitment to secure data connectivity ensures that organizations can share information while maintaining compliance with privacy regulations.
- Cost and Resource Constraints: The financial burden of implementing interoperable systems can be substantial. Organizations often face prohibitive costs associated with technology upgrades and staff training, which can deter them from pursuing necessary improvements. Avato’s solutions are designed to simplify these processes, providing cost-effective pathways to achieving interoperability in healthcare.
Addressing these challenges requires a collaborative effort among all participants in the healthcare ecosystem, including providers, individuals receiving care, technology developers, and regulatory bodies. For instance, the case study titled “Collective Action for Interoperability” illustrates how collaboration among these groups can lead to the establishment of standards that enhance data exchange, improve patient care, and ensure data security and privacy.
Industry leaders emphasize the importance of addressing these barriers. As one representative observed, the national initiative arising from the Cures Act, referred to as TEFCA (Trusted Exchange and Common Agreement Framework), intends to broaden the extent of health information exchange, emphasizing the necessity for coordinated efforts to address connectivity challenges.
Moreover, results from Koldby et al explored the incorporation of a digital dictation system into an EHR, indicating enhancements in workflow while also highlighting problems such as system lockups and inadequate compatibility that restricted advantages.
In summary, while the path to achieving interoperability in medical services is laden with obstacles, the collective action of stakeholders, supported by Avato’s pioneering hybrid integration solutions and the essential role of XML technologies in information transformation, can pave the way for a more connected and efficient system.
Technological Solutions for Interoperability: The Role of FHIR
Fast Healthcare Interoperability Resources (FHIR) represents a transformative standard developed by HL7, designed to simplify the exchange of medical data. By leveraging contemporary web technologies, such as JSON, FHIR facilitates the creation of applications that can seamlessly interact with healthcare information. The lightweight structure of JSON offers significant advantages over XML, particularly in reducing markup overhead and enhancing interchange efficiency, making it an ideal choice for integration platforms that prioritize speed and simplicity.
Why should organizations consider JSON for their data interchange needs? According to user manuals, JSON is essential in scenarios where lightweight information interchange is critical, especially in environments where performance and speed are paramount.
For example, FHIR enables mobile health applications to securely access patient records, greatly enhancing patient engagement and care management. As the healthcare sector evolves, FHIR emerges as a vital enabler of interoperability, effectively dismantling information silos and improving the overall quality of care.
Current adoption rates of FHIR among medical organizations are on the rise, with numerous institutions recognizing its potential to enhance information exchange. A recent study revealed that organizations implementing FHIR reported improved efficiency in data-sharing processes, resulting in better patient outcomes and reduced operational costs. Furthermore, specialists, including integration architects, have noted that FHIR’s adaptability and scalability make it an indispensable resource for modern medical systems.
Dawn Thomas, Integration Architect at UConn Health, remarked, “We put millions of transactions through Cloverleaf and it just runs. For a clinical integration engine, Cloverleaf is robust, scalable, flexible and reliable. You won’t get that from anyone else.”
As we look toward 2025, the latest developments in FHIR technology continue to advance, with ongoing enhancements aimed at further simplifying interoperability challenges in healthcare. Case studies from medical organizations that have successfully implemented FHIR illustrate its effectiveness in improving care coordination and information accessibility. Avato’s hybrid integration platform addresses the challenges of connecting isolated legacy systems and fragmented information, ensuring 24/7 availability for critical integrations.
These advancements underscore FHIR’s pivotal role in transforming medical data exchange, ensuring that care providers can deliver timely and efficient support to patients. Moreover, the sustained use of HL7 V2 in the EHR landscape highlights FHIR’s significance in the current interoperability environment as organizations transition towards more effective information exchange methods. The integration of Procedure Supply Planning further demonstrates how interoperability solutions can enhance patient outcomes and reduce costs, reinforcing the practical benefits of adopting FHIR.
In practical terms, code snippets that illustrate the use of JSON in FHIR implementations can clarify how to effectively utilize this format for information interchange. Additionally, the durability and robustness of XML technologies remain critical, as they guarantee that information remains accessible and usable despite technological shifts, making XML a reliable choice for organizations focused on long-term information management.
Navigating Regulatory Requirements for Healthcare Interoperability
Healthcare institutions face a complex regulatory environment that is crucial for achieving seamless integration. Key regulations, including the Health Insurance Portability and Accountability Act (HIPAA) and the 21st Century Cures Act, impose stringent requirements for information sharing and individual privacy. Compliance with these regulations is essential not only to avoid substantial penalties but also to maintain patient trust and protect sensitive information.
As organizations approach 2025, they must remain vigilant regarding evolving regulations that impact interoperability, such as the Office of the National Coordinator for Health Information Technology (ONC)’s Interoperability Rule. This rule mandates the adoption of standardized information formats, which are vital for smooth information exchange across diverse medical systems. By proactively understanding and adhering to these regulatory frameworks, medical service providers can facilitate smoother information exchanges while ensuring compliance. Furthermore, establishing strong vendor partnerships with technology suppliers is critical for effectively implementing compliant solutions that adapt to these changing regulations.
Avato exemplifies how skilled integration partners can enhance interoperability with its expert integration services and dedicated hybrid integration platform. Their global team ensures that healthcare entities have access to the resources necessary for efficient information integration, enabling the generation of business value by unlocking isolated assets. Avato’s hybrid integration platform streamlines the connection of various systems, aiding organizations in navigating intricate information environments.
For instance, strategic collaborations like those formed by Qualifacts demonstrate how profound integrations can enhance offerings and support compliance initiatives. Their One integration layer facilitates secure data flow across connected solutions, earning praise from clients for its scalability and ability to drive data-informed decision-making.
Expert insights underscore the importance of effectively navigating these regulatory requirements. Compliance specialists emphasize that understanding the definition of interoperability in healthcare and the implications of HIPAA and the 21st Century Cures Act is crucial for medical organizations aiming to improve interoperability.
Statistics reveal that a significant number of medical organizations continue to struggle with compliance challenges, highlighting the urgent need for robust strategies to meet these regulatory demands. Additionally, the World Health Assembly’s resolution WHA71.7 on digital health, adopted in 2018, reinforces the global commitment to enhancing medical interoperability.
Moreover, leveraging technology, including AI, presents opportunities to streamline compliance processes, enhance analytics-driven strategies, and improve fraud detection. By prioritizing compliance and utilizing advanced technology, medical organizations can not only meet regulatory requirements but also elevate their operational capabilities and patient care outcomes. Avato’s integration services provide transparency regarding integration expenses and timelines, enabling organizations to plan efficiently for their integration projects.
Future Trends in Healthcare Interoperability
The future of interoperability in healthcare is set to undergo transformative advancements, primarily driven by emerging technologies. Key trends shaping this evolution include:
- Increased Adoption of FHIR: The Fast Healthcare Interoperability Resources (FHIR) standard is gaining traction as organizations increasingly recognize its potential to facilitate seamless data exchanges. Currently, more than 90% of significant Electronic Health Record (EHR) systems have adopted FHIR APIs, with approximately 64% of U.S. medical providers actively utilizing FHIR. This trend is expected to continue, propelled by regulatory pressures and the necessity for improved health outcomes. The adoption of FHIR has surged due to its ability to enhance interoperability in healthcare, with potential savings projected at $30 billion annually, underscoring its substantial impact on medical efficiency and patient empowerment.
- Integration of AI and Machine Learning: The integration of artificial intelligence and machine learning into medical interoperability is revolutionizing analytical capabilities. These technologies enable predictive analytics, resulting in personalized medicine and more effective care for individuals. As healthcare organizations embrace these innovations, they will enhance their ability to analyze vast amounts of health information, ultimately improving decision-making processes.
- Focus on Individual-Centric Interoperability: Future interoperability initiatives will increasingly prioritize individual engagement. By empowering individuals to access and manage their medical information, providers can foster a more collaborative atmosphere. This shift not only boosts patient satisfaction but also encourages proactive health management.
- Regulatory Evolution: As the healthcare landscape evolves, so too will the regulatory framework governing information exchange and connectivity. Ongoing regulatory changes will promote greater collaboration among healthcare entities, ensuring that data flows seamlessly across systems.
- Reliability in Integration: Avato’s commitment to ensuring 24/7 availability for essential integrations underscores the importance of reliability in healthcare integration solutions. As noted by customer Gustavo Estrada, ‘Avatar has simplified complex projects and delivered results within desired time frames and budget constraints,’ which is crucial for organizations striving to achieve interoperability in healthcare efficiently and effectively.
By proactively embracing these trends, healthcare organizations can position themselves for success in an increasingly interconnected environment, ultimately leading to improved operational efficiency and enhanced patient care. Avato’s hybrid integration platform plays a pivotal role in this transformation, streamlining digital transformation through structured requirements management and modernizing legacy systems in regulated industries. To learn more about how Avato can assist your organization in navigating these changes, download our resources or subscribe to the Avato Blog.
Conclusion
Interoperability in healthcare is vital for improving patient care and operational efficiency. It enables seamless data exchange among various systems, ensuring that patient information is readily accessible and actionable. The importance of foundational, structural, and semantic interoperability cannot be overstated; these elements enhance communication among healthcare providers and lead to better health outcomes.
However, achieving interoperability is fraught with challenges. A lack of standardization, reliance on legacy systems, and complex regulatory requirements hinder progress. These obstacles underscore the necessity for collaboration among all healthcare stakeholders. Organizations like Avato are addressing these challenges by providing hybrid integration solutions that streamline data environments and improve operational visibility.
Looking ahead, the future of healthcare interoperability appears promising. The increasing adoption of standards like FHIR and the integration of artificial intelligence are set to facilitate better data sharing. These advancements will empower patients by granting them greater control over their health information. As healthcare organizations embrace these innovations, they will not only enhance patient care but also navigate a complex regulatory landscape.
In conclusion, prioritizing interoperability is essential for creating a more connected and efficient healthcare system. By overcoming existing challenges and leveraging technology, healthcare providers can unlock the potential of data exchange. This, in turn, leads to improved patient experiences and outcomes. A steadfast commitment to interoperability will be crucial for shaping the future of healthcare.

