Overview
We recognize that effective healthcare connectivity hinges on robust interoperability solutions. In today’s complex healthcare landscape, the ability to seamlessly integrate systems is not just beneficial; it is essential. Our focus is on comparing healthcare interoperability companies to identify solutions that truly enhance connectivity.
We emphasize key features such as:
- Adherence to information exchange standards
- Real-time access
- User-friendly interfaces
- Strong security measures
These elements collectively improve care coordination and operational efficiency in healthcare settings.
What’s holding your team back from achieving optimal integration? By prioritizing these solutions, we can enhance collaboration and ultimately improve patient outcomes. Together, let’s explore how these integration platforms can transform your healthcare delivery. The time to act is now—let us guide you toward effective solutions that meet your needs.
Introduction
In the rapidly evolving landscape of healthcare, interoperability emerges as a critical pillar for enhancing patient care and operational efficiency. We recognize that as healthcare providers strive to share vital patient information seamlessly, understanding the nuances of interoperability is essential. This article delves into the multifaceted nature of healthcare interoperability, exploring its key features, benefits, and the challenges organizations face in achieving effective integration.
What’s holding your team back from realizing the full potential of electronic health information exchange? With statistics revealing significant gaps in this area, the urgency for robust solutions is more pressing than ever. Through real-world examples and expert insights, we highlight how innovative platforms can transform healthcare delivery, ultimately leading to improved outcomes for patients and providers alike.
Understanding Healthcare Interoperability
Healthcare connectivity is vital; it represents the capacity of various information systems, devices, and applications to access, exchange, integrate, and utilize information collaboratively. This capability is crucial for us as healthcare providers to share individual information seamlessly, ultimately leading to improved outcomes and enhanced care coordination. Interoperability is typically categorized into four levels: foundational, structural, semantic, and organizational.
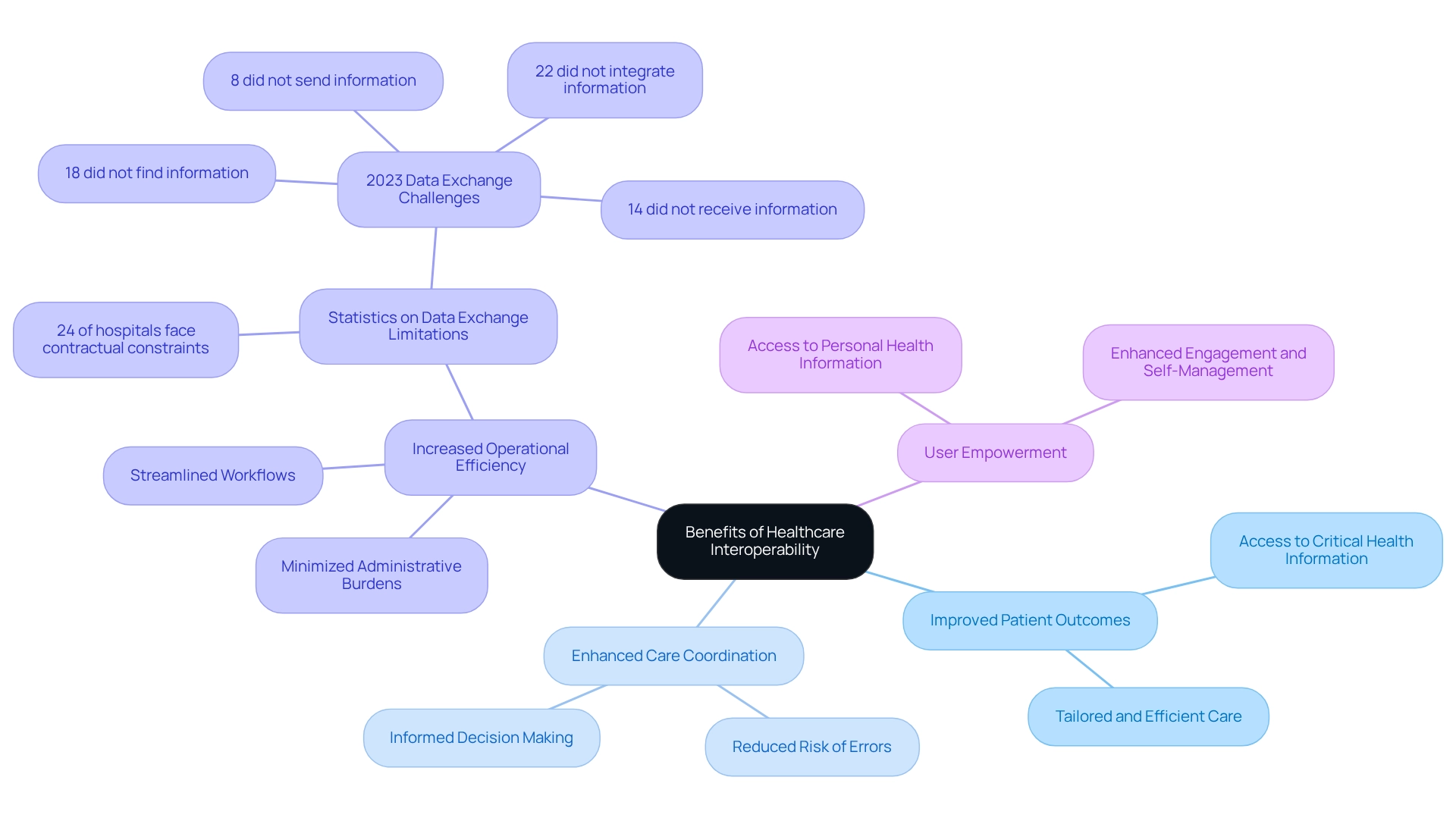
Each level signifies a distinct degree of data sharing and integration capabilities, essential for evaluating interoperability solutions. Recent statistics reveal that 22% of hospitals did not integrate electronic health information in 2023, highlighting ongoing challenges in achieving comprehensive interoperability. This statistic underscores the necessity for strong integration solutions, as the absence of integration can impede effective care and operational efficiency. Furthermore, a significant portion of healthcare executives recognizes the necessity of joining Qualified Health Information Networks (QHINs).
Indeed, one-third of Electronic Health Record (EHR) leaders were actively investigating alternatives in 2022, signifying an increasing recognition of the significance of seamless information exchange in improving care for individuals.
Practical applications of seamless information exchange solutions illustrate their effect on health outcomes. For instance, hospitals that successfully integrate electronic health records can significantly improve care coordination, reduce errors, and enhance patient safety. A logistic regression analysis of hospital attributes has demonstrated that elements like size and ownership impact involvement in health IT surveys, which subsequently influences integration efforts. Grasping these traits is essential for tackling the obstacles to efficient integration.
As the medical environment changes, ongoing assessment of connectivity will be crucial in guiding advancement and assessing policy effects. Expert opinions emphasize that a common, integrated electronic health record is essential for achieving true interoperability. This is progressively acknowledged as a cornerstone of effective medical service delivery.
Solutions offered by healthcare interoperability companies like Avato, with our dedicated hybrid integration platform and expert integration services, can play a crucial role in overcoming the challenges associated with integration. Our dedication to streamlining varied systems and boosting business value guarantees that medical organizations can adjust and prosper in a swiftly evolving environment.
Key Features of Leading Interoperability Solutions
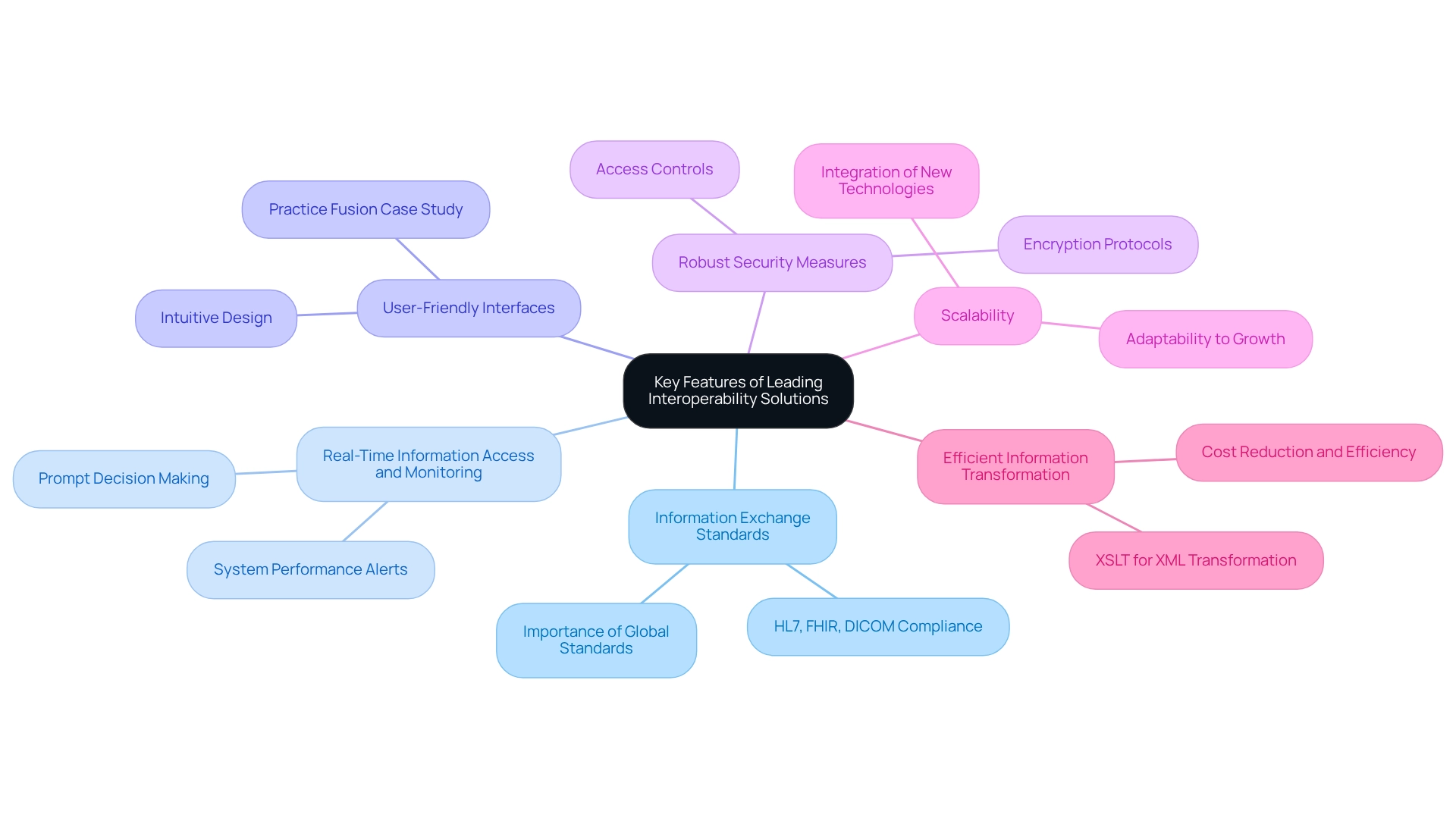
Key Features of Leading Interoperability Solutions
At the forefront of medical innovation, leading interoperability solutions are defined by several essential characteristics that significantly enhance their effectiveness in medical environments:
- Information Exchange Standards: We recognize that adherence to established standards such as HL7, FHIR, and DICOM is crucial for seamless sharing across diverse systems. This ensures that information is transmitted accurately and without loss. As emphasized by Oracle Cerner, compliance with global medical standards is essential for successful integration.
- Real-Time Information Access and Monitoring: Solutions that empower real-time access to individual information enable us to make prompt, informed decisions, significantly enhancing outcomes for individuals. Moreover, real-time monitoring and alerts on system performance are vital for maintaining operational efficiency. Jason Szczuka highlights that enhancing digital wellness entails providing care in more accessible and interconnected methods, underscoring the importance of immediate information access.
- User-Friendly Interfaces: We understand that intuitive interfaces are essential for encouraging uptake among medical personnel. A user-friendly design minimizes training time and enhances operational efficiency. For instance, Practice Fusion has demonstrated how its user-friendly interface improves clinical efficiency and patient involvement, making it a practical option for smaller practices.
- Robust Security Measures: Given the sensitive nature of medical information, we prioritize strong security protocols—including encryption and strict access controls—to safeguard patient details from breaches.
- Scalability: We recognize the capacity to scale solutions in response to organizational growth or the introduction of new technologies is crucial for ensuring long-term viability and adaptability in a rapidly changing medical landscape.
Healthcare interoperability companies must provide effective interoperability solutions that seamlessly integrate with existing systems, including Electronic Health Records (EHRs), laboratory systems, and billing software, to create a cohesive medical ecosystem. Our Hybrid Integration Platform excels in this area, allowing organizations to maximize and extend the value of legacy systems while simplifying complex integrations and significantly lowering costs.
- Efficient Information Transformation: Utilizing XSLT for XML information transformation is a key feature that enhances our integration projects. XSLT’s capability to remove labor-intensive tasks and lessen programming mistakes via schema validation results in significant cost reductions and enhanced efficiency in information management.
As the medical sector continues to progress, the significance of these attributes cannot be overstated. Recent legislation aimed at improving medical IT and tackling information blocking emphasizes the necessity for adherence to exchange standards promoted by healthcare interoperability companies. For instance, specific stipulations in the legislation concentrate on enhancing information accessibility and integration, further highlighting the importance of these solutions in contemporary medical service provision.
Benefits of Healthcare Interoperability
The advantages of medical system interoperability are not just beneficial; they are transformative. We understand that smooth access to comprehensive individual information empowers medical providers to deliver tailored and efficient care. For instance, hospitals that have embraced interoperable systems report significant improvements in patient outcomes, as they can quickly access critical health information across diverse care settings. Our hybrid integration platform, Avato, plays a pivotal role in this process by unlocking isolated assets, facilitating effortless access and sharing of essential information.
Furthermore, interoperability enhances care coordination. By fostering improved communication among providers, we significantly reduce the risk of errors and bolster safety for individuals. This is especially vital in complex cases involving multiple specialists, ensuring that all parties have the necessary information to make informed decisions. Our solutions are designed for secure transactions, making them a trusted choice for healthcare organizations aiming to facilitate this crucial communication.
In addition, we recognize that increased operational efficiency is paramount. By streamlining workflows and minimizing administrative burdens, healthcare organizations can operate more effectively, ultimately reducing costs. A recent study revealed that 24% of hospitals encounter contractual limitations that hinder information exchange, leading to delays in care and increased operational expenses. Our robust solutions from healthcare interoperability companies are essential in overcoming these barriers, enabling organizations to simplify, standardize, and modernize their operations. With support for 12 levels of interface maturity, Avato allows medical providers to balance integration speed with the complexity necessary to future-proof their technology framework.
Moreover, efficient information management is critical for ensuring accuracy and compliance with regulations. Interoperable systems empower organizations to uphold high standards of data integrity, which is essential in today’s regulatory landscape. Our platform supports 12 levels of interface maturity, allowing healthcare providers to balance integration speed with the sophistication needed to future-proof their technology stack.
We also believe in empowering individuals through interoperability. By providing users with easy access to their health information, we enhance engagement and promote self-management of health, leading to better adherence to treatment plans and improved health outcomes. Our commitment to offering a connected framework ensures that individuals can access their information effortlessly. Healthcare leaders emphasize the importance of leveraging integration from healthcare interoperability companies to enhance care for individuals. As Sara Vaezy noted, it’s about applying lessons learned to advance the health system’s mission to serve all patients efficiently and fairly, which is crucial for enhancing connectivity. The ongoing need for comprehensive participation in seamless interactions is underscored by case studies demonstrating that achieving nationwide interoperable exchange requires initiatives like the Trusted Exchange Framework and Common Agreement (TEFCA) to enhance connectivity and mitigate obstacles to information exchange. In 2023, statistics revealed that 8% of hospitals did not send, 18% did not find, 14% did not receive, and 22% did not integrate electronic health information. These figures highlight the pressing need for improvements in system compatibility to enhance care coordination and operational efficiency.
Challenges in Achieving Effective Interoperability
Achieving effective healthcare interoperability is not just beneficial; it is essential. However, the path is fraught with challenges that we must navigate:
- Lack of Standardization: The absence of universally accepted data standards leads to inconsistencies in data exchange, complicating our integration efforts. This lack of standardization presents a significant obstacle, as many medical organizations struggle to implement cohesive interoperability strategies.
- Fragmented Systems: Numerous healthcare organizations operate with disparate systems that fail to communicate effectively, resulting in information silos. This fragmentation hampers operational efficiency and restricts our ability to deliver comprehensive healthcare. Our hybrid integration platform addresses this issue by unlocking isolated assets, enabling seamless connectivity between systems and enhancing overall operational effectiveness.
- Information Privacy Concerns: The security and confidentiality of sensitive health details during information exchange pose significant challenges, especially with increasing regulatory scrutiny. We must implement robust cybersecurity measures to safeguard patient information. Notably, in 2022, global confidence levels in cybersecurity among healthcare organizations were low, underscoring the urgency of addressing these concerns. Our commitment to secure data connectivity ensures that we can navigate these challenges effectively.
- High Implementation Costs: The financial investment needed for integration solutions can be prohibitive, particularly for smaller practices. Many health systems are planning to increase their expenditures on seamless data exchange by 5 to 20% in 2023, reflecting the growing acknowledgment of its significance—a trend we are prepared to support despite the related costs. This increase highlights the challenges we face in balancing budget constraints with the need for effective integration solutions. Our dedication to simplifying these processes can help mitigate costs while maximizing value.
- Resistance to Change: Cultural opposition within organizations can hinder the adoption of new technologies and processes essential for achieving seamless integration. This resistance often stems from a reluctance to alter established workflows, delaying the integration of innovative solutions. Our team of integration experts is dedicated to guiding organizations through these transitions, ensuring a smoother adoption of necessary changes.
Tackling these obstacles is crucial for healthcare interoperability companies seeking to improve system compatibility. Successful case studies demonstrate that accessible and accurate patient records enable public health officials to analyze health trends effectively, ultimately improving community health outcomes. As Conor Stewart, a research expert covering health & pharmaceuticals in the UK & Europe, noted, “In 2022, a third of EHR executives said they were aware of the need to join a QHIN and were actively exploring options.”
This acknowledgment of connectivity challenges is vital as we progress toward 2025, where overcoming these obstacles will be crucial for achieving the full potential of healthcare integration.
At Avato, which derives its name from the Hungarian word for ‘dedication,’ we embody a commitment to architecting the technology foundation required to power rich, connected customer experiences. Our history of enterprise architects striving for better integration solutions underscores our dedication to simplifying complex interoperability challenges. Furthermore, our hybrid integration platform not only addresses current challenges but also positions organizations to future-proof their operations through seamless data and system integration, leveraging XML technologies for effective data transformation.
Conclusion
Healthcare interoperability is not just beneficial; it is essential for enhancing patient care and operational efficiency. By grasping its four levels—foundational, structural, semantic, and organizational—we can assess our integration capabilities and identify areas in need of improvement. Current statistics reveal significant gaps in electronic health information exchange, underscoring the urgent need for effective interoperability solutions that enhance patient outcomes and care coordination.
The benefits of interoperability are manifold, including seamless access to vital health information, which leads to improved patient care and enhanced operational efficiency through streamlined workflows. Furthermore, interoperability empowers patients to manage their health effectively. Key features such as user-friendly interfaces, robust security measures, and scalability are crucial for successful implementation in a rapidly evolving healthcare landscape.
However, challenges persist, including:
- A lack of standardization
- Fragmented systems
- Data privacy concerns
- High implementation costs
- Resistance to change
Addressing these barriers is vital for unlocking interoperability’s full potential. Companies like Avato play a crucial role in providing innovative solutions that simplify integration challenges while ensuring secure data exchange.
In conclusion, achieving effective healthcare interoperability is critical for advancing patient care and operational efficiency. By overcoming existing challenges and adopting robust integration solutions, we can foster a more connected ecosystem, ultimately leading to improved health outcomes for all. What steps will you take to enhance interoperability in your organization?

