Overview
Interoperability in healthcare is not just a technical requirement; it is essential for transforming patient care. The ability of diverse information systems and applications to communicate and exchange patient information seamlessly is crucial for enhancing patient care and reducing medical errors.
We recognize that achieving interoperability involves navigating significant challenges, including:
- Standardization
- Security concerns
- Fragmented systems
Furthermore, we emphasize the importance of collaboration and innovative technological solutions in improving healthcare delivery and patient outcomes.
What’s holding your team back from embracing these advancements? Together, we can address these challenges and pave the way for a more integrated healthcare landscape.
Introduction
In the rapidly evolving landscape of healthcare, we recognize that interoperability is a cornerstone for enhancing patient care and operational efficiency. Defined as the ability of diverse information systems to communicate and exchange data seamlessly, interoperability is essential for healthcare providers striving to deliver coordinated and informed treatment.
With studies revealing that a lack of interoperability contributes to a staggering 30% of medical errors, the urgency to address this challenge is clear. As we increasingly adopt electronic health records and digital tools, understanding the various levels of interoperability—from foundational to organizational—becomes crucial in navigating the complexities of data sharing.
Yet, significant barriers remain, including:
- Standardization issues
- Data privacy concerns
- Resistance to change
This article delves into the importance of interoperability in healthcare, the challenges it faces, and the innovative solutions we are implementing to overcome these hurdles, ultimately aiming to transform patient outcomes and streamline healthcare delivery.
Define Interoperability in Healthcare
Interoperability in medical services is not just a technical requirement; it is the cornerstone of effective healthcare delivery. It embodies the ability of diverse information systems, devices, and applications to communicate, exchange, and utilize information seamlessly. This capability is essential for us as medical providers, enabling smooth access to and sharing of patient information across various technologies and platforms. The significance of seamless integration lies in its power to enhance patient care through a coordinated treatment strategy, which is vital for informed decision-making based on comprehensive patient information. As HIMSS emphasizes, the ability of health information technology (HIT) systems to operate across organizational boundaries not only improves care delivery but also elevates patient outcomes.
Surveys indicate that health leaders globally recognize the critical need to address system compatibility and information standards to fully leverage health information. This awareness underscores the vital role of system compatibility in enhancing healthcare delivery. Daniel Barchi has noted that the industry is currently in the ‘Ford Fairlane’ phase of development regarding system compatibility. This observation suggests that while we have made initial progress, significant challenges remain before we achieve complete integration and functionality.
Moreover, expert insights highlight the necessity for robust big data solutions to effectively evaluate and analyze compatibility issues. This is crucial to mitigate biases in design and execution, as no single organization can tackle the complexities of system compatibility alone. Successful collaborations within medical networks demonstrate the potential to improve patient outcomes and streamline processes, establishing collaboration as a fundamental aspect of modern medicine. Additionally, the ongoing maintenance of integrated Clinical Decision Support tools is essential to ensure their functionality as electronic health records (EHRs) evolve, emphasizing the continuous effort required to sustain compatibility. Enhancing FHIR adoption for clinical decision support tools is a pivotal step towards better connectivity, facilitating improved information exchange and utilization across medical platforms.
At Avato, we are dedicated to navigating this landscape by simplifying complex integrations and maximizing the value of legacy systems. Our hybrid integration platform enables secure and seamless connectivity, real-time monitoring, and significant cost savings, empowering medical organizations to overcome interoperability challenges. Our commitment to crafting technological solutions not only enhances operational efficiency but also supports our primary mission: to improve patient care through better information utilization.
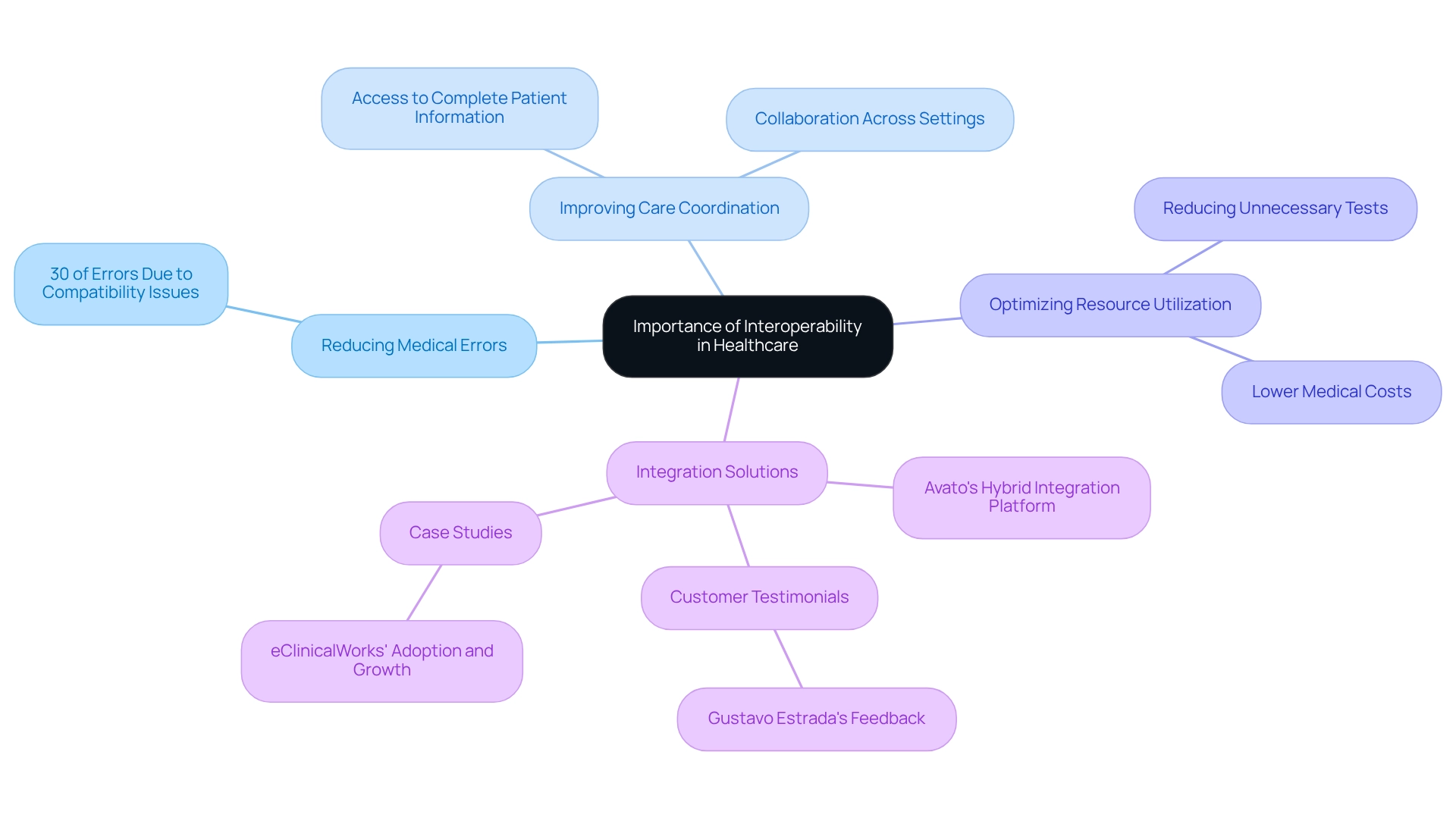
Contextualize the Importance of Interoperability
Understanding interoperability in healthcare is crucial for enhancing the quality of care, as it ensures that we, as providers, have access to complete and accurate patient information. This access significantly mitigates the risk of medical errors, a leading cause of adverse patient outcomes. Research indicates that a lack of system compatibility accounts for approximately 30% of medical mistakes, underscoring the necessity for seamless data exchange among medical networks.
When emergency responders can quickly access a patient’s medical history, they are better equipped to make informed decisions that can save lives. Furthermore, system compatibility fosters improved care coordination, enabling medical professionals to collaborate effectively across various settings. This partnership not only enhances patient outcomes but also optimizes resource utilization by reducing unnecessary tests and procedures, ultimately leading to lower medical costs.
As medical networks increasingly adopt electronic health records (EHRs) and diverse digital tools, the significance of interoperability in healthcare becomes even more pronounced. Our hybrid integration platform at Avato is designed to address these compatibility challenges by providing a robust solution that facilitates secure and efficient information sharing across different systems. This capability is essential for organizations seeking to modernize their operations and elevate patient care.
Moreover, our commitment to simplifying complex integration projects is reflected in customer testimonials, such as that of Gustavo Estrada, who remarked, “Avato has the ability to simplify complex projects and deliver results within desired time frames and budget constraints.” This highlights our role in achieving compatibility through efficient integration solutions tailored for the medical field. By focusing on the specific challenges of interoperability in healthcare, we empower organizations to navigate the complexities of connectivity with confidence, ensuring that improved patient outcomes are not merely an aspiration but a reality.
Explore the Levels of Interoperability
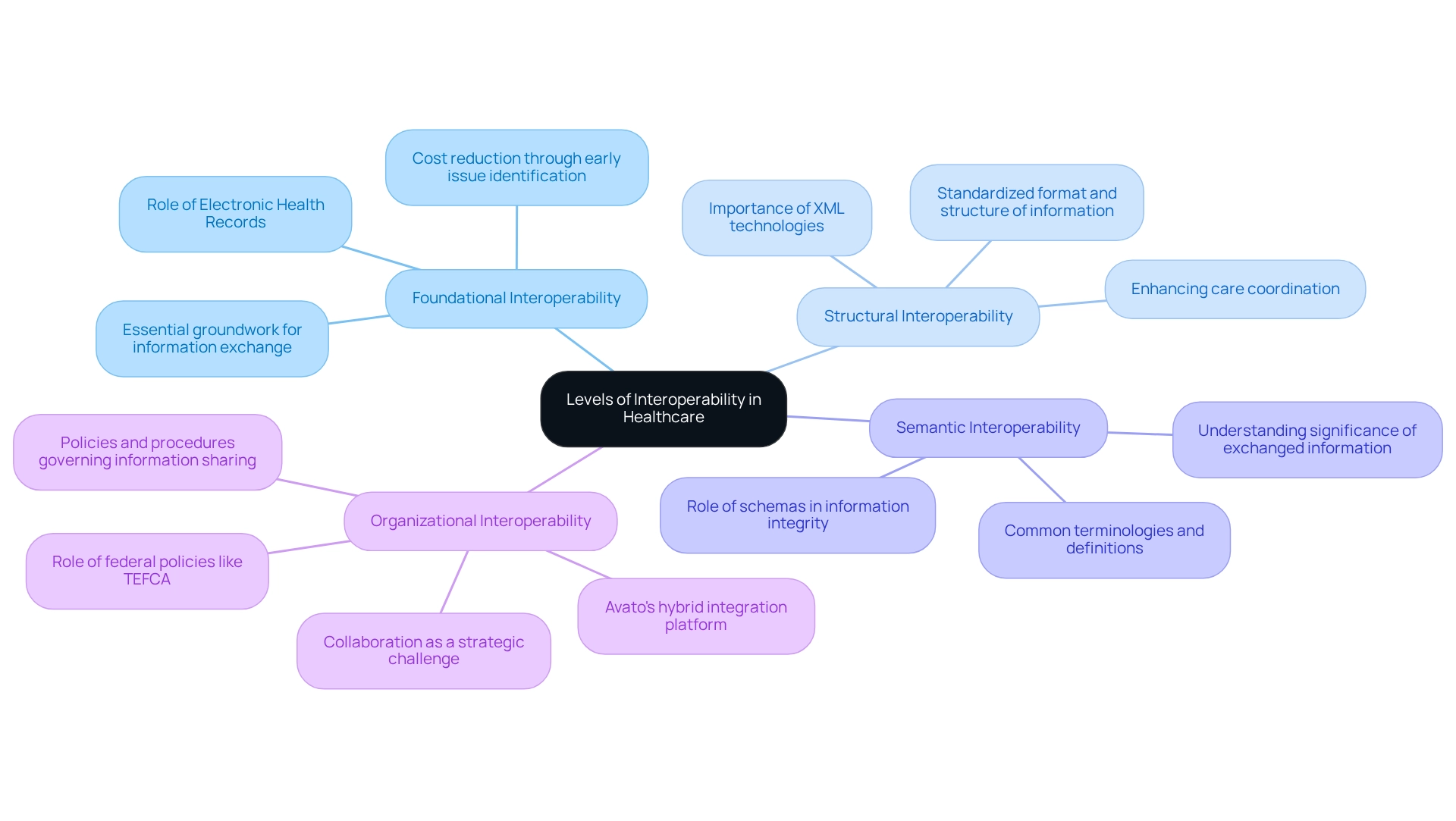
Interoperability in healthcare is a crucial concept that can be understood through four distinct levels: foundational, structural, semantic, and organizational.
Foundational Interoperability represents the essential groundwork for effective information exchange, allowing one system to send information to another without requiring the receiving system to comprehend it. A common, integrated electronic health record serves as the foundation for achieving interoperability, as highlighted by Mera Choi, Director of the Technical Strategy and Analysis Division. Implementing schemas at this level can significantly reduce costs related to errors, as identifying issues early in information entry is far less expensive than rectifying them later, which may lead to costly decisions based on incorrect information.
Structural Interoperability defines the format and structure of information, enabling networks to exchange details in a standardized manner. This ensures that the information can be accurately interpreted by the receiving system, enhancing clarity and usability. For instance, standardized formats like XML facilitate the sharing of patient details among various healthcare providers, improving care coordination. The application of XML technologies is vital for ensuring that information remains interoperable and accessible over time, which is critical for integration projects.
Semantic Interoperability takes this a step further by ensuring that both systems understand the significance of the exchanged information. This relies on common terminologies and definitions, promoting a more meaningful and context-aware exchange. Such understanding is essential for healthcare providers to interpret and utilize information effectively in clinical decision-making. The role of schemas here is paramount, as they help preserve the integrity and longevity of the information exchanged.
Organizational Interoperability represents the highest level, encompassing the policies and procedures that govern information sharing and usage across different organizations. This level underscores that collaboration is not merely a technical challenge; it is a strategic one, necessitating cooperation and consensus among various stakeholders. Federal policies and initiatives, such as the Trusted Exchange Framework and Common Agreement (TEFCA), are pivotal in enhancing seamless communication by mitigating barriers to information exchange. Avato’s hybrid integration platform exemplifies how organizations can streamline the unification of disparate systems, ultimately enhancing business value and fostering collaboration through specialized solutions.
Understanding these tiers is essential for medical organizations aiming to enhance their collaborative capabilities, as each level builds upon the previous one to create a unified and effective data exchange environment. However, challenges remain, including the lack of incentives and alignment of stakeholder interests, which can hinder collaboration and obstruct seamless integration initiatives. Addressing these challenges is crucial for unlocking the full potential of health IT tools in transforming healthcare services.
Identify Challenges in Achieving Interoperability
Understanding interoperability in healthcare presents numerous challenges that we must navigate effectively. The key barriers include:
- Lack of Standardization: The absence of consistent information formats and structures across healthcare organizations complicates seamless information sharing, leading to inefficiencies. Our hybrid integration platform, developed from a strong commitment to simplifying integration challenges, tackles this issue by enabling the connection of diverse systems, facilitating smoother exchanges of information.
- Information Privacy and Security Concerns: Safeguarding patient information during exchanges is paramount. Organizations face the dual challenge of adhering to stringent regulations while implementing robust security measures to protect sensitive information. As Robin Leahy, Vice President of Compliance, highlights, understanding what interoperability means in healthcare is critical, emphasizing the need for secure information exchanges. Our solutions are crafted with security as a priority, ensuring that information integrity is upheld during the integration process.
- Fragmented Systems and Data Silos: Many medical providers depend on isolated systems that do not communicate, leading to data silos that impede effective information flow and obstruct patient care. For example, PaceMate’s Remote Cardiac Monitoring Solution illustrates how seamless collaboration can improve patient care. Similarly, our specialized integration services assist organizations in accessing these separate resources, fostering a more interconnected medical environment through our global network of integration partners.
- Resistance to Change: Healthcare professionals often hesitate to embrace new technologies or processes, especially when accustomed to conventional methods, which can hinder advancement toward system compatibility. Our dedicated team of integration specialists offers essential assistance to facilitate this transition, ensuring that medical organizations can adjust to new frameworks efficiently.
- Integration Costs: The financial consequences of merging different systems can be overwhelming, particularly for smaller entities, establishing a significant obstacle to achieving seamless operations. We provide customized solutions that can help reduce these expenses, making integration more accessible for all medical providers.
Moreover, as of 2022, 50% of medical organizations performed regular cybersecurity audits, indicating the industry’s increasing awareness of data privacy issues and the necessity for robust security measures amid integration challenges. Understanding interoperability in healthcare is crucial for comprehensive measurement, informing progress, and evaluating policy impacts, ultimately paving the way for a more interconnected healthcare landscape.
Conclusion
Interoperability in healthcare is not merely a technical necessity; it is a crucial element in enhancing patient care and operational efficiency. The ability of diverse information systems to communicate effectively can significantly reduce medical errors, which currently account for approximately 30% of such incidents. This underscores the urgent need for seamless data sharing among healthcare providers. With our increasing reliance on electronic health records and digital tools, the importance of interoperability has never been more pronounced.
The journey toward achieving interoperability is complex, involving various levels that range from foundational to organizational. Each level builds on the previous one, creating a robust framework for data exchange that enhances care coordination and decision-making. We must address challenges such as lack of standardization, data privacy concerns, and resistance to change to unlock the full potential of health IT tools in transforming healthcare delivery.
Innovative solutions, such as Avato’s hybrid integration platform, are paving the way for overcoming these barriers. By simplifying complex integrations and ensuring secure data exchange, these tools not only promote operational efficiency but also prioritize patient outcomes. As the healthcare landscape continues to evolve, our commitment to interoperability will be crucial in fostering collaboration among stakeholders and ultimately delivering high-quality care.
In conclusion, the path toward achieving interoperability is essential for a more connected and efficient healthcare system. By recognizing the importance of seamless data sharing and actively addressing the challenges that hinder progress, we can enhance patient outcomes and streamline operations. The future of healthcare depends on the successful implementation of interoperability, making it a priority for all stakeholders involved.

