Overview
EHR interoperability is crucial for the seamless communication and exchange of patient information across various electronic health record systems. This capability is essential for enhancing care coordination and improving patient outcomes. Effective interoperability not only reduces medical errors but also fosters patient-centered care. Supported by compelling statistics, the significant use of certified health IT in hospitals demonstrates successful implementations that lead to improved patient safety and operational efficiency.
As healthcare professionals, how can we leverage this integration to address our current challenges? By embracing EHR interoperability, we can ensure that patient information flows effortlessly between systems, ultimately enhancing the quality of care we provide. The evidence is clear: a robust interoperability framework is not just beneficial; it is imperative for the future of healthcare. Let’s take action to integrate these systems and witness the transformative impact on patient care.
Introduction
In the rapidly evolving landscape of healthcare, the ability of electronic health record (EHR) systems to seamlessly communicate and exchange patient information has emerged as a cornerstone of effective patient care. EHR interoperability is not merely a technical requirement; it is a critical enabler of enhanced care coordination, reduced medical errors, and improved patient outcomes. As healthcare providers strive to deliver patient-centered care, understanding the intricacies of EHR interoperability becomes paramount.
Furthermore, with the introduction of frameworks like the Trusted Exchange Framework and Common Agreement (TEFCA), organizations are now better equipped to navigate the complexities of data sharing. This article delves into the definition, significance, levels, benefits, challenges, and future trends of EHR interoperability. Are you ready to explore its transformative potential in shaping a more connected and efficient healthcare system?
Understanding EHR Interoperability: Definition and Significance
What is EHR interoperability? It is defined as the capability of various electronic health record (EHR) systems to communicate, exchange, and utilize patient information seamlessly. This functionality is crucial as it enables healthcare providers to access a comprehensive view of patient data, irrespective of the care settings involved. Effective collaboration not only enhances care coordination but also plays a vital role in reducing medical errors and improving overall patient outcomes.
As of 2025, the significance of EHR connectivity has become even more pronounced, with healthcare leaders emphasizing its role in fostering patient-centered care. A recent review emphasizes that EHR integration significantly contributes to patient safety, medication safety, and overall healthcare efficiency. The Trusted Exchange Framework and Common Agreement (TEFCA), launched in 2022, seeks to create a nationwide network for the secure and seamless sharing of healthcare information, further enhancing cooperation across the healthcare field by offering a standardized method for information exchange.
Statistics indicate that as of 2016, over 95% of eligible and Critical Access hospitals have shown significant use of certified health IT, highlighting the broad acknowledgment of EHR compatibility’s advantages. Successful implementations in hospitals have illustrated its positive impact on patient outcomes, with studies indicating that integrated EHR systems can lead to lower rates of adverse clinical events, particularly in vulnerable populations such as patients with diabetes. For instance, the study by Reed et al. analyzed the rates of negative clinical occurrences in individuals with diabetes 30 days following release from the hospital utilizing a new shared, integrated electronic health record, emphasizing the essential role of connected systems in improving patient safety.
Furthermore, an extensive evaluation of 12 studies concerning electronic health record connectivity showed variability in information reliability, with seven studies assessed as low risk. This highlights the significance of strong collaborative frameworks in ensuring high-quality information exchange and patient safety. Avato’s hybrid integration platform plays a crucial role in this landscape by maximizing the value of legacy technologies, simplifying complex integrations, and providing real-time monitoring and alerts on performance.
By tackling the issues of system compatibility, Avato ensures that healthcare organizations can efficiently access data and systems while significantly lowering costs. As healthcare continues to progress, understanding what EHR interoperability is and its application will be crucial for organizations aiming to provide high-quality services and enhance patient care.

Levels of EHR Interoperability: From Foundational to Semantic
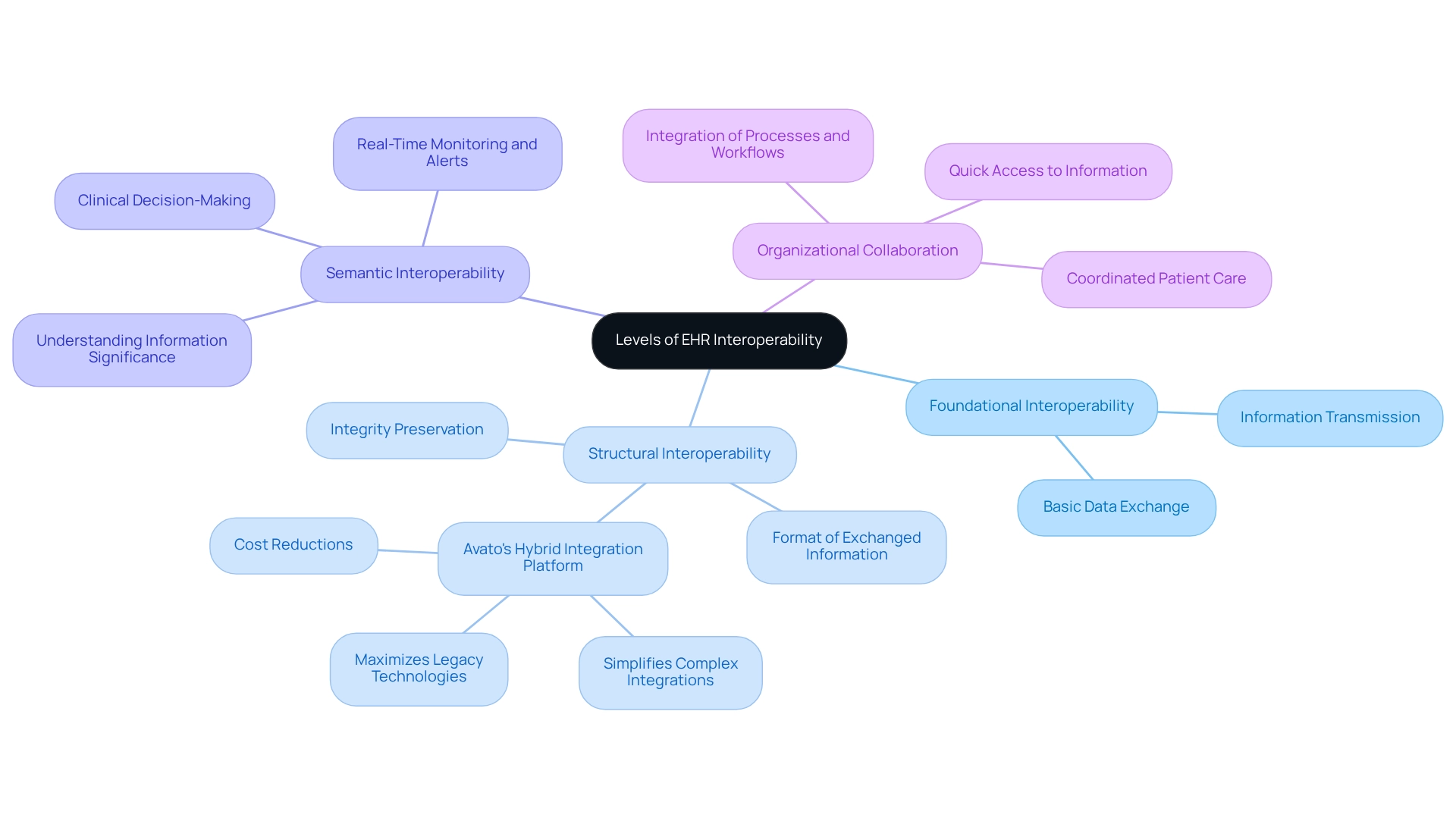
Understanding EHR interoperability is crucial for effective healthcare delivery, categorized into four primary levels: foundational, structural, semantic, and organizational.
Foundational Interoperability is the most fundamental level, allowing one network to transmit information to another. While it ensures that information can be received, it does not guarantee that the receiving apparatus can interpret the content accurately.
Structural Interoperability defines the format of exchanged information, ensuring that the receiving framework can accurately interpret the details. This is vital for preserving integrity during transfers, a capability that Avato’s Hybrid Integration Platform enhances by simplifying complex integrations and maximizing the value of legacy technologies, ultimately leading to substantial cost reductions.
Semantic Interoperability surpasses simple information exchange; it guarantees that frameworks comprehend the significance of the information being shared. This understanding is vital for effective clinical decision-making, allowing healthcare providers to interpret patient information accurately and make informed choices. Avato’s platform facilitates this by offering real-time monitoring and alerts on system performance, ensuring that information remains actionable and pertinent.
Organizational Collaboration represents the highest level of collaboration, integrating processes and workflows across different organizations. This facilitates smooth collaboration and information sharing, crucial for coordinated patient care. With Avato’s secure hybrid integration features, organizations can access information and networks in weeks, not months, enabling quicker and more effective healthcare delivery.
Understanding EHR interoperability is essential for healthcare organizations aiming to improve their connectivity capabilities. As of 2025, the adoption of EHR integration has advanced significantly, with statistics indicating that EHR implementation has reduced the time required to access patient information by up to 80%. Furthermore, the 21st Century Cures Act Final Rule, enacted in 2023, has been pivotal in advancing seamless data exchange and preventing information obstruction in EHR frameworks, aligning with Avato’s dedication to improving connectivity and adherence.
Expert perspectives emphasize the importance of foundational, structural, semantic, and organizational connectivity in achieving extensive data sharing and enhancing patient outcomes. For instance, a recent study on the creation of a multidisciplinary hand-over information framework demonstrated that effective communication among medical team members could be greatly improved through organized collaboration practices. Over two years, this initiative prepared more than 40 seed anchors, highlighting the practical implications of these connection levels in real-world healthcare environments.
Moreover, compared to a current paper-based Kardex system, nurses reported a 50% reduction in time, further demonstrating the efficiency improvements from enhanced collaboration. In the competitive ambulatory EHR market, firms such as Epic, Cerner, and MEDITECH lead the way, with Epic holding a 33.4% market share, underscoring the industry’s emphasis on improving collaborative efforts. The essential role of XML in ensuring data compatibility and longevity for integration projects cannot be overlooked, as it provides a robust framework for data sharing that remains relevant across technological advancements.
Key Benefits of EHR Interoperability in Healthcare
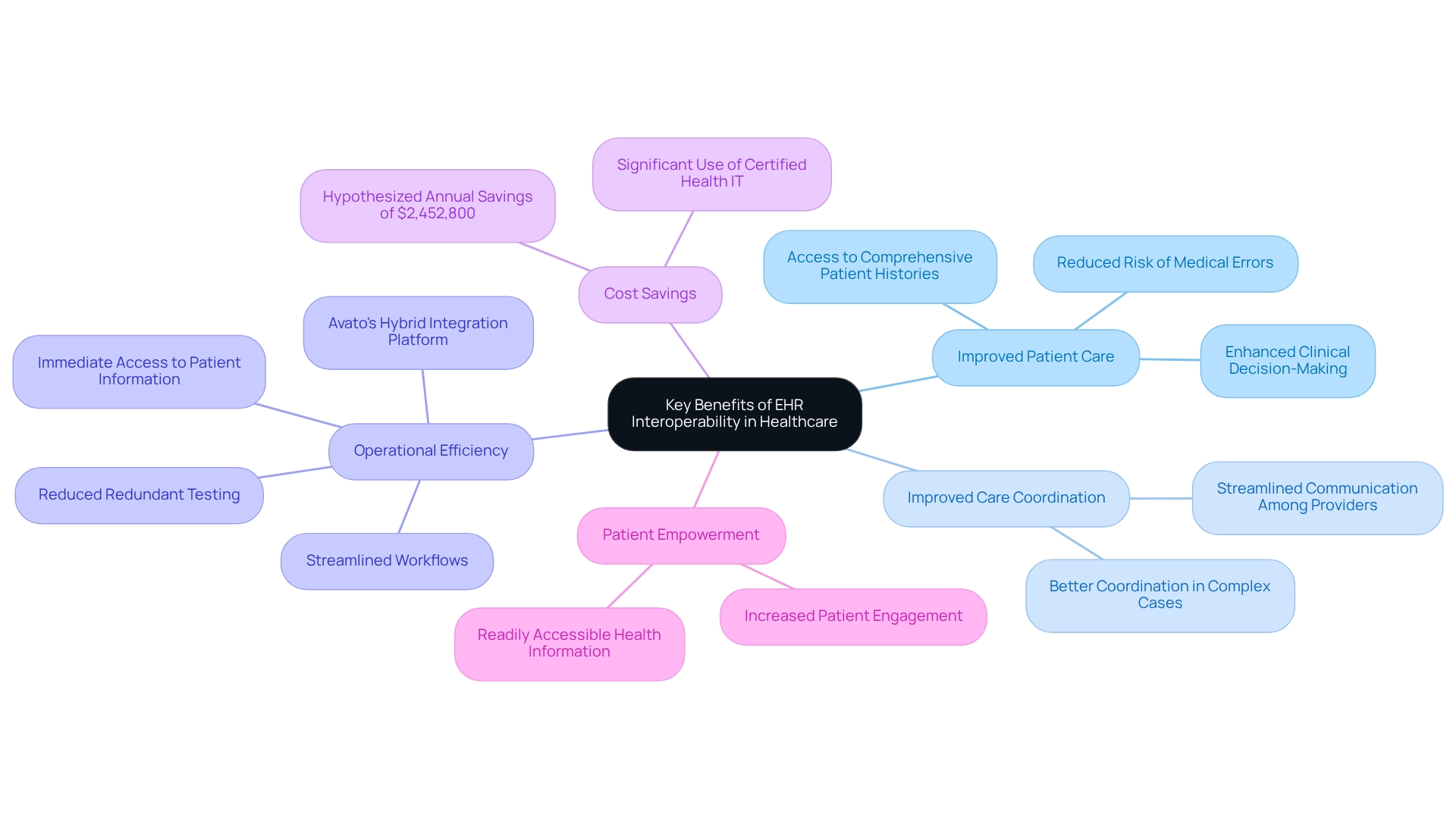
The advantages of EHR interoperability in healthcare are extensive and impactful:
- Improved Patient Care: Interoperability empowers healthcare providers to access comprehensive patient histories. This access significantly reduces the risk of medical errors and enhances clinical decision-making, which is crucial for delivering accurate diagnoses and effective treatments.
- Improved Care Coordination: Integrated platforms streamline communication among healthcare providers, fostering better coordination and efficiency in care delivery. This is particularly vital in complex cases involving multiple specialists, ensuring that all parties remain informed and aligned.
- Operational Efficiency: Organizations benefit from streamlined workflows and reduced redundant testing. Immediate access to patient information minimizes delays, saving time and optimizing resource allocation. This allows healthcare professionals to focus more on patient care. Avato’s hybrid integration platform plays an essential role by unlocking isolated assets and facilitating smooth information flow across networks. Tony Leblanc from the Provincial Health Services Authority noted, “Avato accelerates the integration of isolated systems and fragmented data, delivering the connected foundation enterprises need to simplify, standardize, and modernize.”
- Cost Savings: The financial consequences of system compatibility are significant. By minimizing errors and enhancing operational efficiency, healthcare organizations can achieve substantial cost reductions. A study hypothesized annual savings of approximately $2,452,800 due to decreased documentation times for nurses, illustrating the economic benefits of improved workflows. Furthermore, as of 2016, over 95% of qualified and Critical Access hospitals exhibited significant use of certified health IT by engaging in CMS EHR Incentive Programs, emphasizing the broad acknowledgment of its value. Avato’s platform specifically contributes to these savings by providing 12 levels of interface maturity, allowing organizations to balance speed of integration with the sophistication required to future-proof their technology stack.
- Patient Empowerment: Patients benefit from having their health information readily accessible, which encourages greater engagement in their care. This empowerment leads to better health outcomes, as informed patients are more likely to adhere to treatment plans and participate actively in their health management.
These advantages underscore the crucial function of collaboration in contemporary healthcare frameworks, particularly in understanding EHR interoperability as the sector progresses towards more unified and patient-focused care models. As of 2025, the focus on seamless integration continues to expand, with healthcare professionals increasingly acknowledging EHR interoperability and its potential to enhance care coordination and improve patient outcomes. A recent study, “Assessing the Effectiveness of a New Medical Records Transfer Process,” evaluated an innovative workflow implemented during the COVID-19 pandemic, revealing favorable responses from staff and efficient information transfer across a three-hospital network, highlighting the practical benefits of integration in real-world environments.
Moreover, in 2022, a third of EHR leaders recognized the necessity to join a QHIN and were actively investigating alternatives, as highlighted by research specialist Conor Stewart. This demonstrates a proactive strategy to improve connectivity in healthcare. Avato’s commitment to architecting the technology foundation necessary for these advancements ensures that organizations can navigate the complexities of integration with confidence.
Challenges and Barriers to EHR Interoperability
Achieving EHR interoperability presents significant challenges that must be addressed for healthcare organizations to collaborate effectively.
- Lack of Standardization: The diversity in EHR systems often leads to varied data formats and terminologies, complicating seamless information sharing. This inconsistency hinders effective communication between healthcare providers, ultimately impacting patient care. Avato’s hybrid integration platform effectively tackles this issue by providing tools that standardize data formats, facilitating smoother information exchange.
- High Implementation Costs: Enhancing current setups and educating staff incurs considerable financial consequences. Many organizations find the costs associated with implementing EHR integration solutions to be excessive, hindering progress toward cohesive healthcare systems. Avato’s solutions are designed to enhance integration strategies, assisting organizations in managing expenses while achieving compatibility.
- Privacy and Security Concerns: Safeguarding patient information during transmission is crucial. Organizations frequently express concerns about potential breaches that could expose sensitive information, leading to reluctance in fully embracing interoperability initiatives. Avato prioritizes security in its integration processes, ensuring that data remains protected throughout its lifecycle.
- Resistance to Change: Healthcare providers often hesitate to embrace new structures or processes, particularly when they are comfortable with existing workflows. This resistance can slow the transition to more interoperable solutions, despite long-term benefits. Avato’s dedicated team collaborates closely with stakeholders to mobilize them and model new business processes, easing the transition and fostering acceptance of new technologies.
- Regulatory Barriers: Navigating the complex landscape of healthcare regulations complicates interoperability efforts. Organizations must ensure adherence to various legal requirements, creating additional obstacles in their pursuit of integrated solutions. Avato assists organizations in preparing for the future by incorporating compliance factors into their solutions, simplifying the regulatory navigation process.
Tackling these challenges is essential for healthcare organizations striving to enhance EHR interoperability. Recent discussions among healthcare leaders underscore the urgency of overcoming these barriers to realize the full potential of EHR systems. The ONC’s forecast that genuine integration would be accomplished between 2021 and 2024 highlights this urgency.
Moreover, case studies focusing on patient perspectives on EHR compatibility emphasize the importance of considering user experiences in the evaluation process. Future research should address not only the technical aspects but also the positive and negative impacts of interoperable EHR interventions from the patient’s viewpoint, ensuring that their needs are prioritized. As Gustavo Estrada from BC Provincial Health Services Authority stated, “Avato has the capability to simplify intricate projects and produce outcomes within preferred timelines and financial limitations,” emphasizing the significance of effective solutions in addressing these integration challenges.
Additionally, the call for the creation of shared health information technology research outcome measures is vital for improving the quality of upcoming studies on EHR compatibility.
Best Practices for Achieving EHR Interoperability
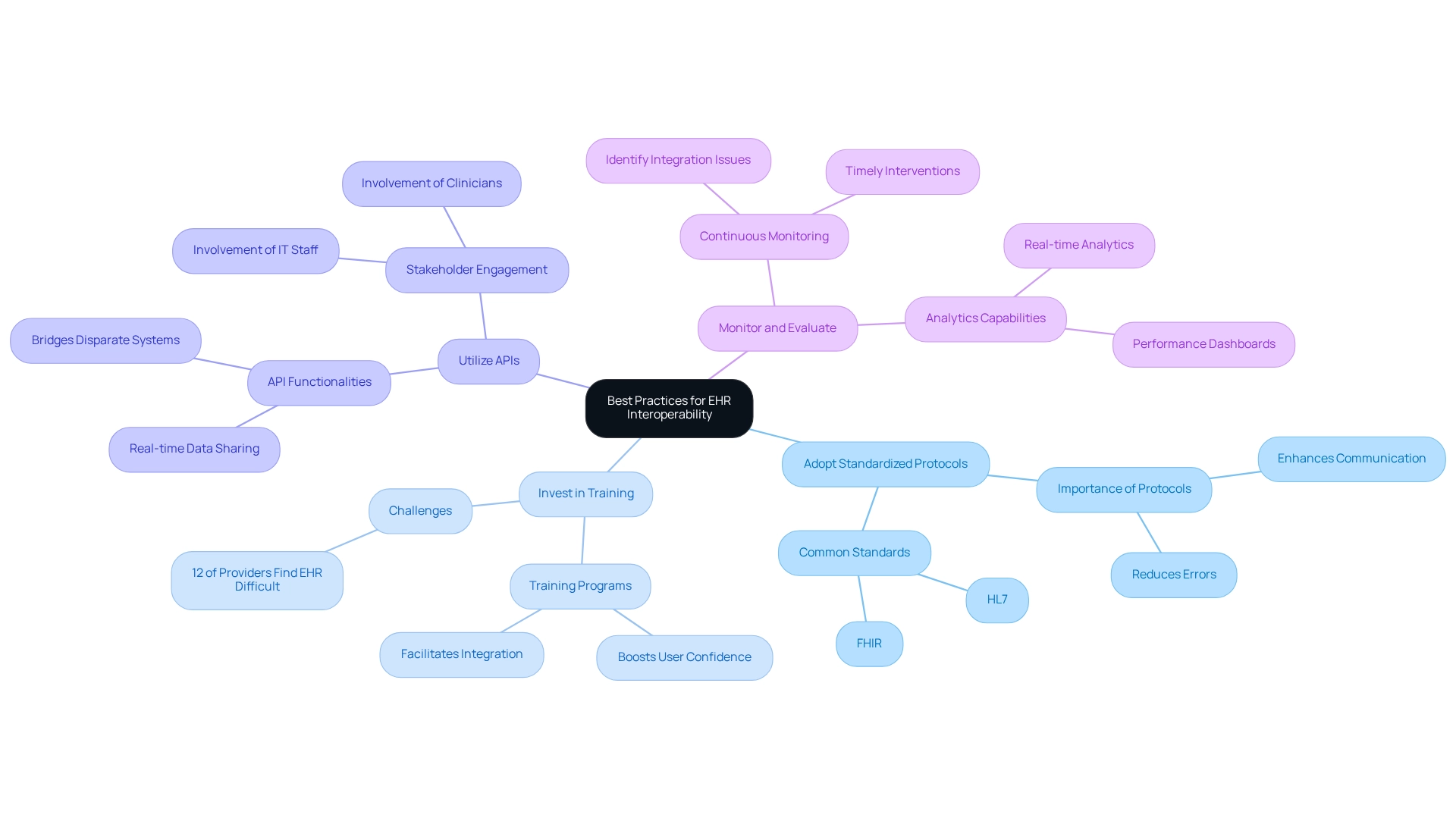
To effectively achieve EHR compatibility, healthcare organizations must consider the following best practices:
-
Adopt Standardized Protocols: Employing common information standards, such as HL7 and FHIR, is crucial for enabling smoother information exchange between platforms. The impact of standardized protocols on EHR interoperability success cannot be overstated; they provide a framework that enhances communication and reduces errors in information management. Understanding EHR interoperability can significantly improve data quality and minimize mistakes, which is essential for enhancing patient care.
-
Invest in Training: Ensuring that personnel are well-trained in new methods and procedures is vital for successful implementation. Effective training programs not only boost user confidence but also facilitate a more seamless integration of EHR platforms. Given that 12% of providers find their EHR somewhat challenging to use, addressing training needs is essential.
-
Utilize APIs: Implementing application programming interfaces (APIs) can greatly enhance the ability of various platforms to communicate effectively. APIs act as bridges that allow disparate systems to share data in real-time, which is vital for improving patient care and operational efficiency, especially when considering EHR interoperability. Engaging stakeholders, including clinicians and IT staff, in the planning and implementation process is key to addressing concerns and fostering buy-in. This collaborative approach ensures that the needs of all stakeholders are considered, resulting in more effective solutions.
-
Monitor and Evaluate: Regularly reviewing collaborative efforts and making necessary modifications can assist organizations in staying on track and achieving their objectives. Continuous monitoring, supported by robust analytics capabilities, allows for the early identification of integration issues, enabling timely interventions that can enhance overall performance. This is where Avato’s hybrid integration platform excels, offering features like real-time analytics and performance dashboards that provide the insights necessary to optimize operations and enhance customer experiences.
By adhering to these best practices, healthcare organizations can significantly improve their connectivity capabilities, which is essential for understanding EHR interoperability, ultimately leading to better patient care and operational outcomes. For instance, a study by Koldby et al. highlighted the integration of a digital dictation system into an EHR, resulting in workflow improvements and time savings, despite some noted integration challenges.
This case study illustrates both the potential advantages and drawbacks of collaborative initiatives, underscoring the importance of a strategic approach. Furthermore, Biltoft et al. observed that reducing documentation durations could yield annual savings of US$ 2,452,800, highlighting the financial benefits of efficient collaboration practices.
Real-World Examples of Successful EHR Interoperability
Numerous healthcare organizations have effectively implemented EHR interoperability, showcasing its substantial benefits.
Mayo Clinic achieved remarkable success in care coordination by adopting interoperable systems in 2025. This initiative empowered healthcare providers to access detailed patient information across various facilities, significantly improving patient outcomes. Statistics indicate that this compatibility has led to a notable decrease in hospital readmission rates, underscoring its impact on patient care.
CommonWell Health Alliance is a collaborative initiative designed to enhance information exchange among various EHR systems, ensuring that providers can access patient details regardless of the care environment. By facilitating seamless communication, CommonWell has significantly improved the continuity of care, a crucial element for effective treatment.
Veterans Health Administration (VHA) has made substantial progress in data exchange, enabling seamless information sharing between its facilities and external providers. This integration not only enhances care for veterans but also boosts operational efficiency, illustrating the essential role of system compatibility in modern healthcare.
These examples illustrate the transformative potential of EHR integration in enhancing patient care and operational efficiency, paving the way for a more connected and responsive healthcare system. However, ongoing challenges must be acknowledged. The Academy of Medical Royal Colleges has highlighted a lack of understanding regarding the differences in EHR use between primary and secondary care, indicating a need for further research.
Moreover, a recent analysis revealed that six of the quantitative non-randomized studies achieved a perfect score of 5/5 on the MMAT, indicating a high level of effectiveness in EHR integration initiatives. As Taiwo Adedeji noted, “The ToC applies to the whole life cycle of the intervention from the creation right through to the evaluation,” emphasizing the importance of a comprehensive approach to EHR implementation.
Additionally, the Pilot EHR Implementation at Festac Primary Health Center in Lagos State, Nigeria, serves as a case study that highlights both the challenges and achievements of EHR integration in primary care environments. This pilot initiative laid the groundwork for health information exchange and demonstrated the potential for system integration and clinical decision support, stressing the importance of tailoring implementation processes to local contexts.
For Banking IT Managers, understanding EHR interoperability is crucial, particularly concerning information security and compliance. As healthcare organizations increasingly rely on interconnected networks, the implications for data governance and regulatory compliance become paramount. Avato’s hybrid integration platform plays a vital role in this landscape, enabling secure transactions and facilitating the integration of isolated systems.
By addressing the complexities of EHR integration, Avato empowers healthcare organizations to manage these challenges efficiently, ensuring sustainability and cost reductions while providing a robust foundation for digital transformation efforts.
Future Trends in EHR Interoperability: What to Expect
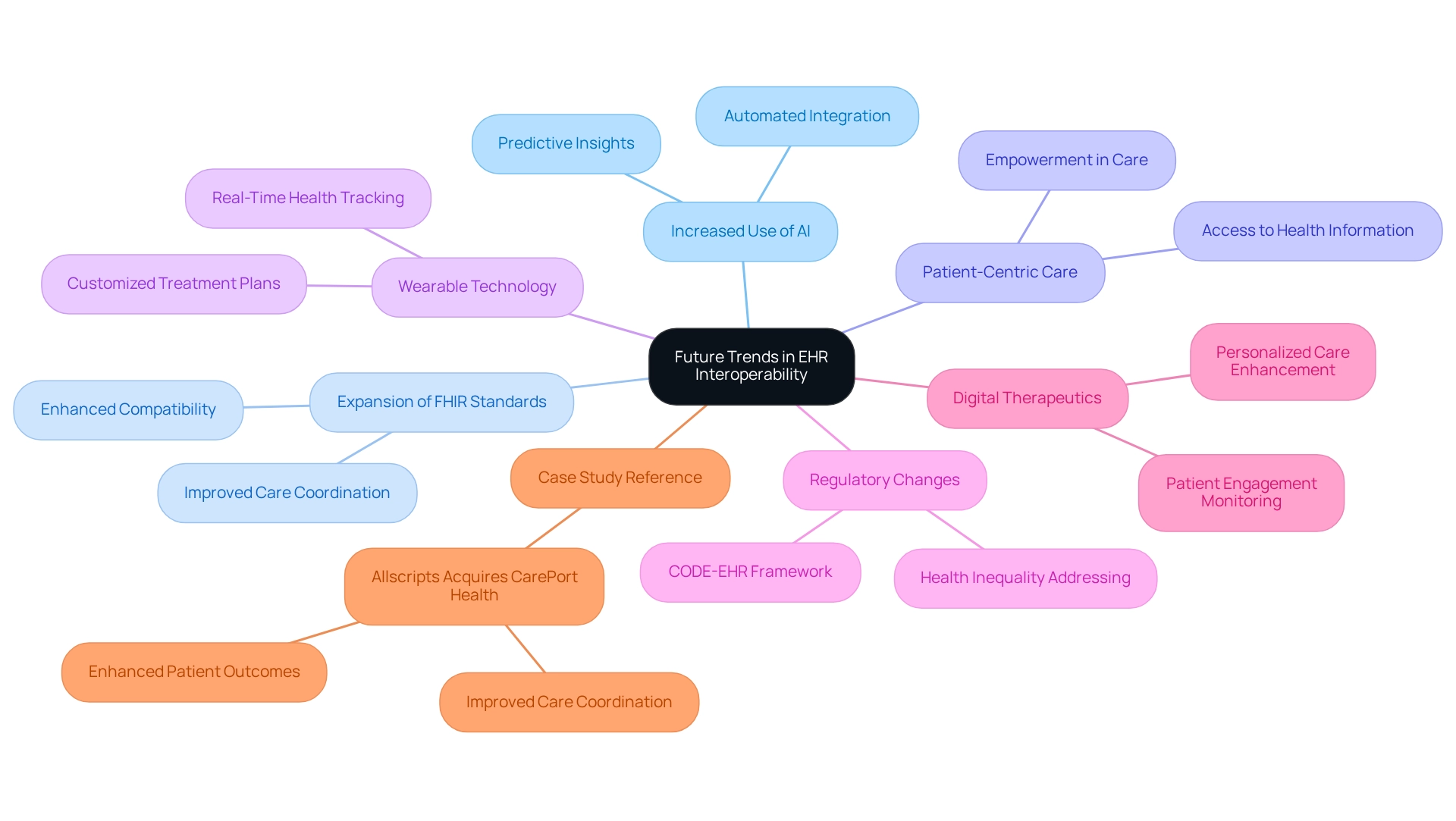
The future of EHR interoperability is poised for transformative advancements, marked by several key trends:
-
Increased Use of Artificial Intelligence: AI is anticipated to revolutionize information analysis and decision-making processes, significantly enhancing the efficiency of interoperability initiatives. By automating information integration and providing predictive insights, AI will streamline workflows and enhance patient outcomes. As Gustavo Estrada observed, Avato streamlines intricate projects and produces outcomes within preferred timelines and financial limitations, highlighting the practical advantages of such progress.
-
Expansion of FHIR Standards: The question of what is EHR interoperability can be addressed by the expectation that the Fast Healthcare Interoperability Resources (FHIR) standard will experience wider acceptance, facilitating more effortless information exchange across various healthcare networks. This standardization will enhance compatibility, allowing for quicker access to patient information and improved care coordination, which is essential for leveraging Avato’s hybrid integration platform.
-
Greater Focus on Patient-Centric Care: As the healthcare landscape shifts towards patient-centered models, compatibility will become increasingly vital. Understanding what is EHR interoperability is crucial for ensuring that patients can access their health information across various providers, empowering them to take an active role in their care and ultimately leading to better health outcomes. Avato’s solutions are intended to improve this patient-focused method by streamlining the connection of various systems.
-
Incorporation of Wearable Technology: The rise of wearable devices will increase the necessity for improved compatibility to include real-time health information into EHR systems. This integration will allow healthcare providers to track patients more effectively and customize treatment plans based on ongoing health metrics, further backed by Avato’s dedicated hybrid integration platform.
-
Regulatory Changes: Ongoing regulatory developments, such as those highlighted by the CODE-EHR framework, will continue to impact what is EHR interoperability, compelling organizations to adopt more robust and compliant solutions. These modifications will not only improve information sharing but also tackle health inequalities by ensuring complete patient information is accessible for informed choices, a goal that aligns with Avato’s mission.
-
Integration of Digital Therapeutics: The incorporation of digital therapeutics with EHRs will enhance personalized care and monitor patient engagement, further underscoring the significance of seamless connectivity in contemporary healthcare. Avato’s platform is crucial in enabling this integration, ensuring smooth information connectivity.
-
Case Study Reference: The recent purchase of CarePort Health by Allscripts for $250 million demonstrates the practical effects of connectivity advancements. This merger aims to enhance care coordination and is anticipated to improve patient outcomes by incorporating CarePort’s solutions with Allscripts’ EHR platforms, demonstrating the real-world effects of efficient integration.
By keeping informed about these trends, healthcare organizations can strategically ready themselves for the changing environment of what is EHR interoperability, ensuring they stay competitive and able to provide high-quality care. Future EHR systems may also include comprehensive data on patients’ social, economic, and environmental conditions to address health disparities, highlighting the evolving nature of data integration and the role of Avato in pioneering these solutions.
Conclusion
EHR interoperability stands as a cornerstone of modern healthcare, significantly enhancing both patient care and operational efficiency. This article underscores its critical role in enabling seamless communication between electronic health record systems, which ultimately leads to improved care coordination, reduced medical errors, and superior patient outcomes.
The various levels of interoperability—foundational, structural, semantic, and organizational—illustrate the intricate nature of achieving effective data exchange. Each level is pivotal in supporting clinical decision-making and ensuring patient safety. Moreover, the advantages of interoperability, including heightened patient engagement and cost savings, underscore its essential role for healthcare organizations.
However, despite these benefits, challenges persist. Issues such as a lack of standardization, high implementation costs, and privacy concerns pose significant barriers to progress. Organizations can navigate these obstacles by adopting best practices, such as engaging stakeholders and providing comprehensive training.
Looking forward, trends like the integration of artificial intelligence, the expansion of FHIR standards, and the utilization of wearable technology are set to propel EHR interoperability to new heights. These innovations will not only empower patients but also enhance care coordination, making it imperative for organizations to embrace these advancements.
In conclusion, prioritizing EHR interoperability is essential for healthcare organizations aiming to deliver high-quality, patient-centered care. By acknowledging its significance and addressing the existing challenges, the healthcare industry can significantly enhance patient outcomes and cultivate a more connected and efficient system for all stakeholders.

