Overview
In today’s rapidly evolving landscape, digital transformation is not just an option; it is a necessity for enhancing healthcare services. Our article, “10 Insights from the Healthcare Digital Transformation Book,” delves into key insights and strategies that can revolutionize patient care and operational efficiency. By leveraging cutting-edge technologies such as AI, telemedicine, and data analytics, we can tackle the pressing challenges faced by the healthcare sector. These innovations hold the potential to significantly improve patient outcomes and sustainability.
What barriers are currently hindering your team’s progress? We invite you to explore how embracing these digital solutions can lead to transformative results in your organization.
Introduction
In the rapidly evolving landscape of healthcare, we recognize that digital transformation stands as a pivotal driver of efficiency, sustainability, and improved patient outcomes. As organizations grapple with the complexities of integrating new technologies, platforms like Avato’s hybrid integration system provide innovative solutions that bridge the gap between legacy systems and modern applications. By enabling seamless data flow and enhancing interoperability, we empower healthcare providers to focus on what truly matters: delivering high-quality patient care.
This article delves into the myriad ways digital innovation is reshaping healthcare, from reducing waste and enhancing operational efficiency to embracing sustainability and overcoming barriers to transformation. As the sector moves toward a more integrated and responsive future, understanding these trends will be crucial for healthcare leaders like you aiming to navigate the digital age successfully.
Avato: Transforming Healthcare with a Secure Hybrid Integration Platform
At Avato, we understand the intricate challenges that medical systems face. Our hybrid integration platform is expertly crafted to securely link disparate technologies, empowering medical organizations to modernize their operations. By facilitating seamless data flow between legacy systems and new applications, we enable healthcare providers to concentrate on patient care rather than technical hurdles. This ultimately enhances health outcomes and operational efficiency.
Consider this: recent data shows that approximately 97% of hospitals and 88% of medical clinics in the U.S. have embraced cloud-based solutions to enhance care quality. Unification and interoperability not only streamline access to records but also highlight the financial advantages of our platform. Furthermore, the U.S. government’s investment in digital wellness initiatives, particularly in electronic health record (EHR) interoperability and telemedicine growth, underscores the increasing significance of unification technology in medical services. By incorporating telemedicine into medical records, we ensure continuity of care, enhancing user engagement and access to healthcare services.
Our hybrid unification platform simplifies complex connection projects while maximizing and extending the value of legacy systems. We deliver results within desired time frames and budget constraints. As Gustavo Estrada, one of our satisfied customers, noted, “Avato has the ability to simplify complex projects and deliver results within desired time frames and budget constraints.” This sentiment reflects our commitment to addressing connectivity challenges, ultimately resulting in enhanced operational productivity and user engagement.
IT leaders in the medical field consistently stress the need for robust unification solutions to navigate the evolving landscape. Trust in Avato as your partner in driving healthcare digital transformation in the medical sector. Together, we can overcome the complexities of integration and focus on what truly matters—improving patient outcomes.
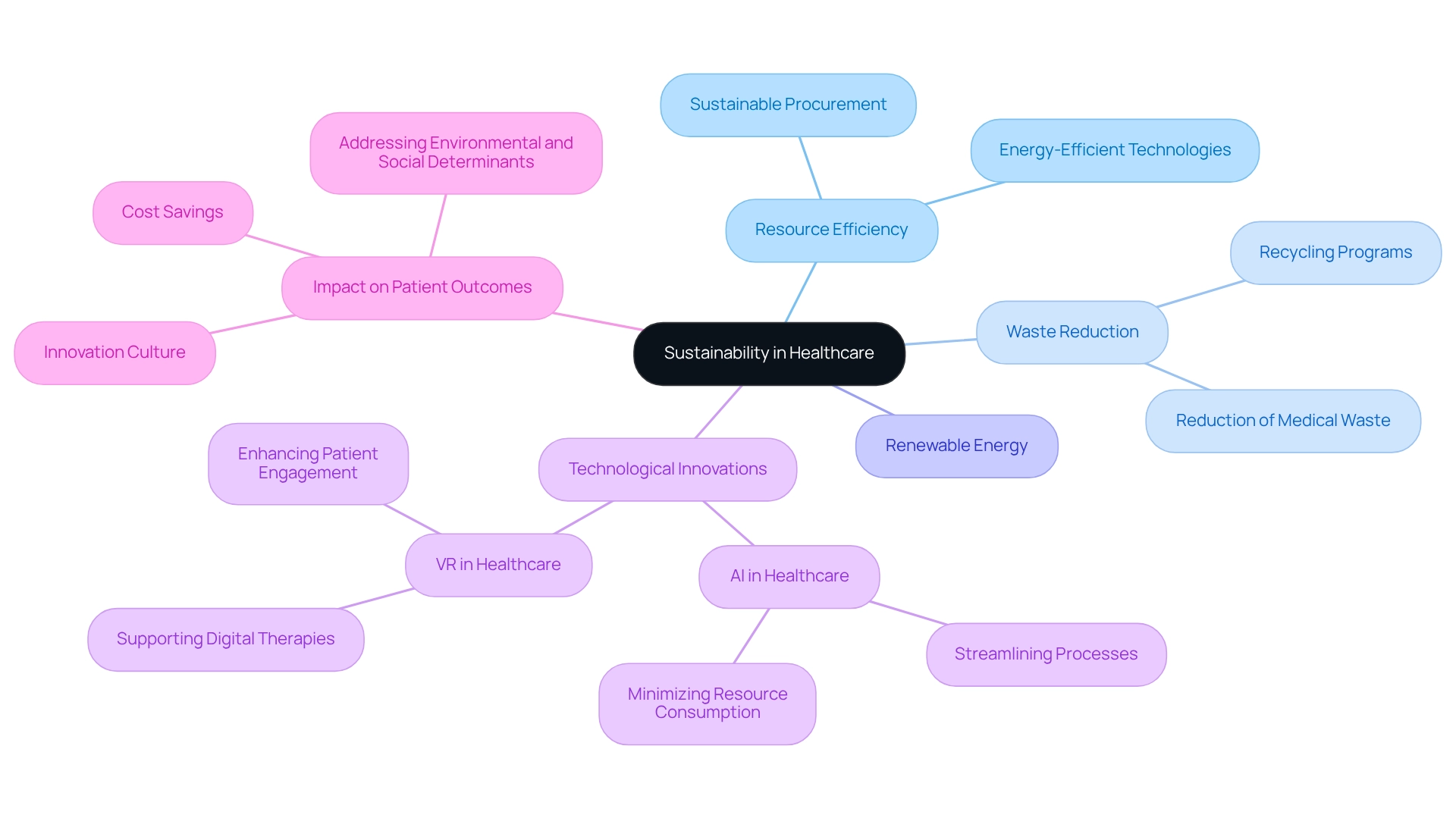
Defining Sustainability in Healthcare: Key Principles and Practices
Sustainability in healthcare is not merely a trend; it is an imperative that we must embrace to reduce environmental impact while ensuring high-quality care for individuals. Our core principles focus on resource efficiency, waste reduction, and the integration of renewable energy sources. We are witnessing a growing trend among healthcare organizations adopting strategies such as:
- Recycling programs
- Sustainable procurement
- Energy-efficient technologies
Notably, the rise of electronic medicine, particularly through AI and VR, serves as a transformative approach that not only enhances patient care but also supports our sustainability objectives. For instance, digital therapies can diminish reliance on pharmaceuticals, thereby lessening waste and the ecological repercussions associated with medication manufacturing and disposal.
As we approach 2025, the medical sector recognizes that sustainable practices are not only beneficial for the environment but also critical for enhancing operational efficiency and reputation. Current statistics indicate that medical waste accounts for approximately 5% of the sector’s total carbon emissions, underscoring the urgent need for organizations to adopt greener practices. By aligning our operational strategies with sustainability goals, we can significantly reduce our carbon footprint while simultaneously improving care and outcomes. The application of AI and VR technologies can streamline processes, minimize resource consumption, and elevate patient engagement, further bolstering our sustainability efforts.
Experts affirm that successful sustainability initiatives can yield substantial cost savings and foster a culture of innovation within medical organizations. Kaiser Permanente exemplifies this success, demonstrating the benefits of integrating sustainability into medical practices. Moreover, sustainable practices are vital for addressing environmental and social determinants of health, highlighting their broader implications. The urgency of implementing sustainable medical practices is paramount for modernizing our systems and enhancing patient outcomes, making it a top priority for medical organizations today.
Reducing Waste in Healthcare: Strategies for Digital Transformation
The healthcare digital transformation book outlines a powerful array of strategies for minimizing waste in healthcare. We recognize that the adoption of electronic health records (EHRs) significantly reduces paper usage, streamlining documentation processes and enhancing overall efficiency. Furthermore, electronic inventory management systems play a crucial role in optimizing supply chain operations, effectively reducing excess stock and waste. Telemedicine also contributes to waste reduction by decreasing the necessity for physical appointments, which in turn lowers transportation-related emissions.
The integration of digital medicine, particularly through the use of artificial intelligence (AI) and virtual reality (VR), is revolutionizing healthcare. For example, our AI-driven avatar, Nadia, can interact with elderly patients, providing personalized advice about their treatments. Meanwhile, VR applications have demonstrated remarkable success in pain management, such as reducing pain perception in children during needle procedures. These technologies not only enhance treatment options but also humanize the medical experience, offering immersive experiences that alleviate distress and improve outcomes.
Data analytics empowers medical organizations to identify waste patterns, enabling them to apply targeted interventions that yield significant cost savings and enhance sustainability. A case study on EHR implementation underscores the potential for these systems to save billions in medical expenses each year, reinforcing the economic rationale for hospitals to invest in advanced EHR functionalities. Our research concluded that advanced EHR functionalities could lead to improved quality, safety for individuals, and clinical efficiencies, with the average adverse incident rate decreasing by 0.03 from 2014 to 2016.
As noted by Soumya Upadhyay, PhD, MHA, “For policymakers, it might be valuable to revisit the meaningful use criteria so that hospitals can perform efficiently regarding improving quality and safety while following this regulation.” This statement emphasizes the critical role of EHRs in enhancing medical quality and safety. Moreover, it is essential for individuals to have ownership and access to their health data, allowing them to explore new treatment options. As the medical field continues to evolve, utilizing insights from the healthcare digital transformation book, particularly the integration of AI and VR, will be vital for achieving operational efficiency and improving care for individuals.
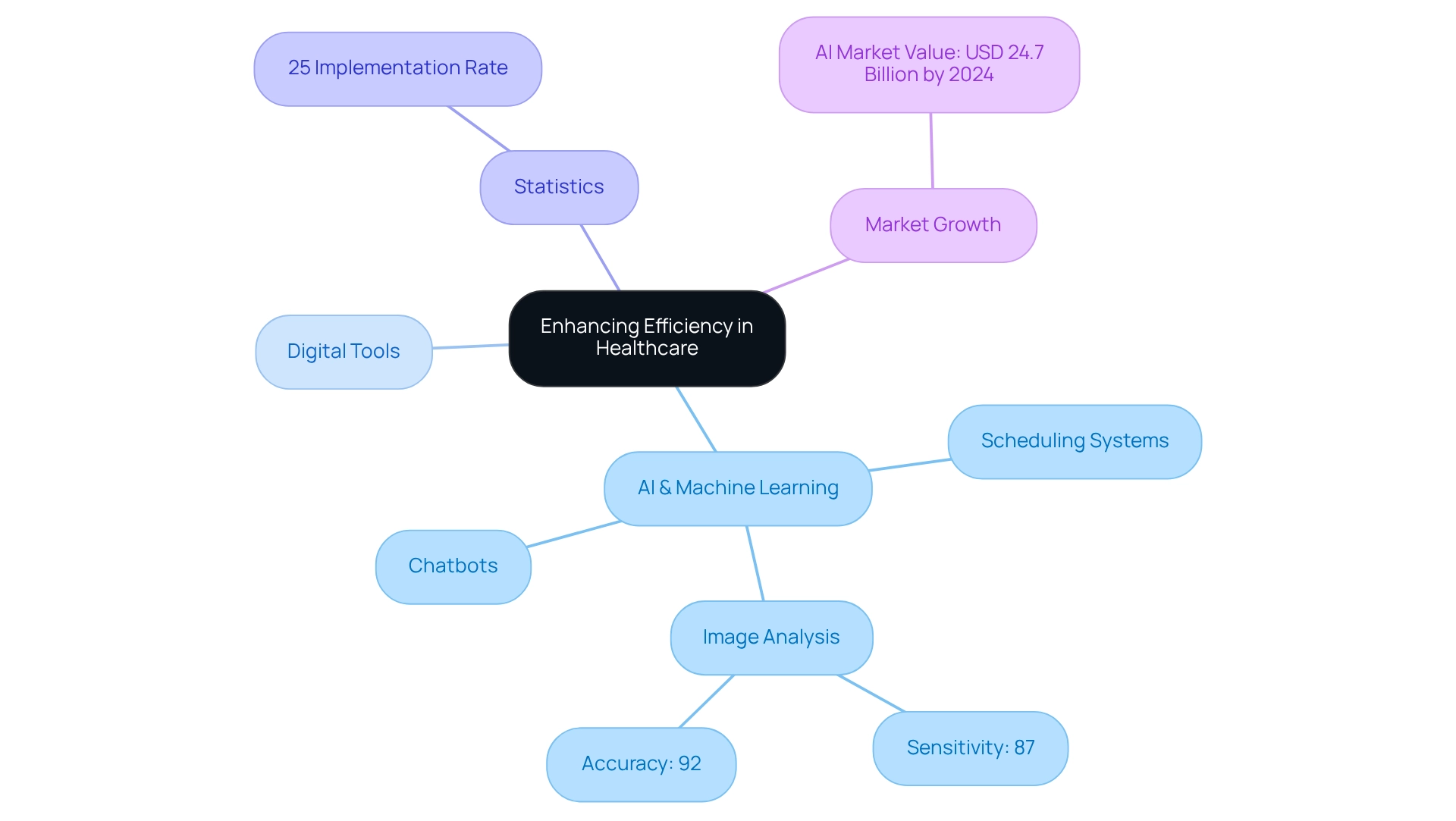
Enhancing Efficiency in Healthcare: The Role of Digital Tools
Digital tools are revolutionizing efficiency in medical systems. We recognize that technologies such as artificial intelligence (AI) and machine learning simplify administrative duties, enabling medical professionals to devote more time to patient care. For instance, AI-driven chatbots adeptly manage routine inquiries, allowing our staff to focus on more complex responsibilities.
Furthermore, digital scheduling systems significantly enhance appointment management, resulting in reduced patient wait times and increased satisfaction. In fact, AI in the medical field is projected to alleviate the burden on professionals by automating various administrative functions, thereby improving overall productivity.
Notably, as of December 2023, only 25% of healthcare executives had implemented generative AI solutions, indicating a substantial opportunity for growth in this area. With machine learning demonstrating 87% sensitivity and 92% accuracy in medical image analysis, the synergy of these technologies not only enhances operational efficiency but also elevates the quality of healthcare.
The application of virtual reality (VR) and AI is transforming patient interactions, offering empathetic support through digital avatars and expanding treatment options. Our Hybrid Integration Platform is pivotal in this transformation, facilitating the seamless integration of these technologies into existing medical systems.
The AI market within the medical field is anticipated to reach approximately USD 24.7 billion by 2024, underscoring the growing significance and investment in AI solutions within the sector. Moreover, emphasizing data accessibility and ownership is crucial; patients must maintain control over their health data to fully leverage these advancements.
As we continue to embrace these innovations, organizations can expect enhanced resource allocation and a more responsive medical environment. For banking IT managers, understanding these advancements is essential, as they may face similar unification challenges and data security concerns when adopting new technologies in their own industry.
Integrating Healthcare Systems: Achieving Seamless Operations
Achieving seamless operations in medical services hinges on the effective integration of diverse systems and technologies. Interoperability is crucial; it allows various medical applications to communicate and share information, which is essential for coordinated patient care. Notably, statistics indicate that 26% of hospitals that occasionally engaged in interoperable exchanges reported that clinicians frequently utilized clinical information available electronically from external providers (Everson J., 2023, Office of the National Coordinator for Health Information Technology). By implementing standards such as HL7 and FHIR, we significantly enhance this integration, enabling care providers to swiftly access comprehensive patient information.
Our current initiatives, including the Trusted Exchange Framework and Common Agreement (TEFCA), aim to bridge interoperability gaps and improve data-sharing capabilities across the care continuum. These efforts highlight the critical role interoperability plays in unlocking the full potential of health IT tools. Our hybrid unification platform exemplifies how organizations can overcome connectivity challenges, ensuring that all systems operate cohesively to improve patient outcomes and optimize operations. By leveraging these standards, we facilitate the implementation of HL7 and FHIR, allowing medical systems to foster a more interconnected and responsive environment. Furthermore, our platform maximizes and extends the value of legacy systems, simplifies complex integrations, and significantly reduces costs. With support for 12 levels of interface maturity, we empower medical organizations to access data and systems in weeks, not months, ultimately enhancing care coordination. Additionally, our platform provides real-time monitoring and notifications regarding system performance, enabling IT managers in the medical sector to maintain operational reliability and proactively address issues.
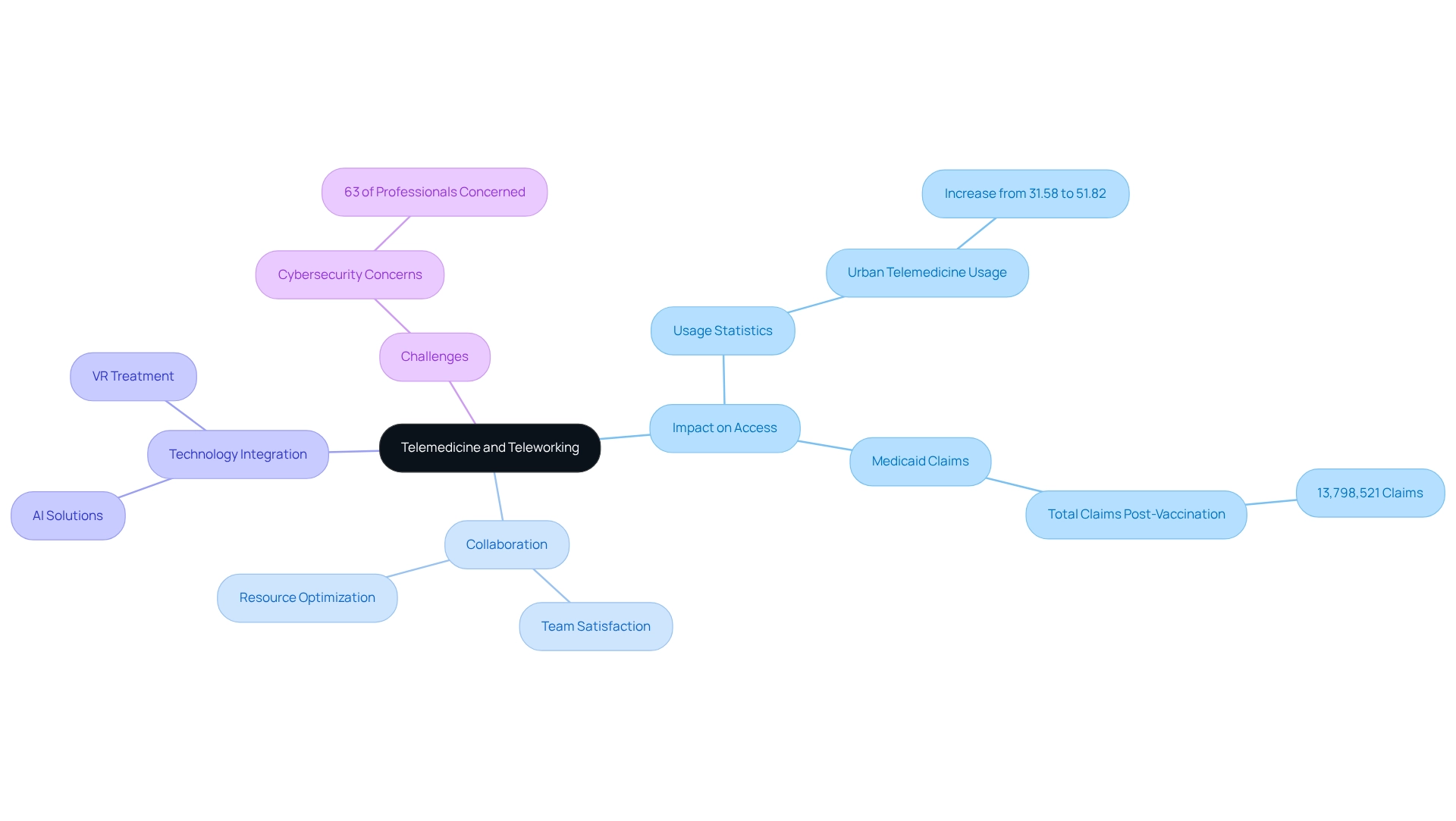
Telemedicine and Teleworking: Revolutionizing Healthcare Delivery
Telemedicine and teleworking have fundamentally transformed medical service delivery, significantly enhancing access to care and alleviating pressure on medical facilities. Virtual consultations empower our patients to receive medical advice from the comfort of their homes—an essential advantage for those in remote areas or facing mobility challenges. This shift has resulted in a remarkable increase in telemedicine adoption, with urban telemedicine usage soaring from 31.58% to 51.82% during the pandemic’s second phase. Furthermore, the total number of Medicaid claims during the pandemic after vaccination reached 13,798,521, underscoring the extensive utilization of telemedicine and its impact on medical service provision.
In addition, teleworking fosters seamless collaboration among medical professionals, regardless of their physical locations. This flexibility not only boosts satisfaction among our team members but also optimizes resource utilization within healthcare systems. For instance, a study on telehealth completion rates revealed significant disparities among individuals with different insurance types, highlighting the necessity for tailored approaches to enhance telemedicine adoption. As Dwight Lewis, PhD, remarked, “Although all services have diminished since their peak in the shutdown period of the second phase of the pandemic, behavioral health, psychologists’ services, and mental health providers showed continued high utilization post-large-scale vaccine availability.”
The integration of digital medicine, particularly through AI and VR, is further revolutionizing healthcare as outlined in the healthcare digital transformation book. Technologies such as virtual reality exhibit remarkable potential in treating conditions like PTSD, enabling individuals to engage with their treatment in immersive environments that can alleviate pain perception and promote recovery. AI-driven solutions are also emerging as trusted advisors, providing our patients with personalized information regarding their treatments and wellness management, thereby humanizing the medical experience.
As we move towards 2025, the telemedicine landscape continues to evolve, with medical leaders recognizing its potential to revolutionize service delivery. However, challenges remain, as 63% of medical professionals express concerns regarding cybersecurity risks associated with cloud-based systems, such as electronic health records. Addressing these challenges will be crucial for preserving the benefits of telemedicine and teleworking in the medical field.
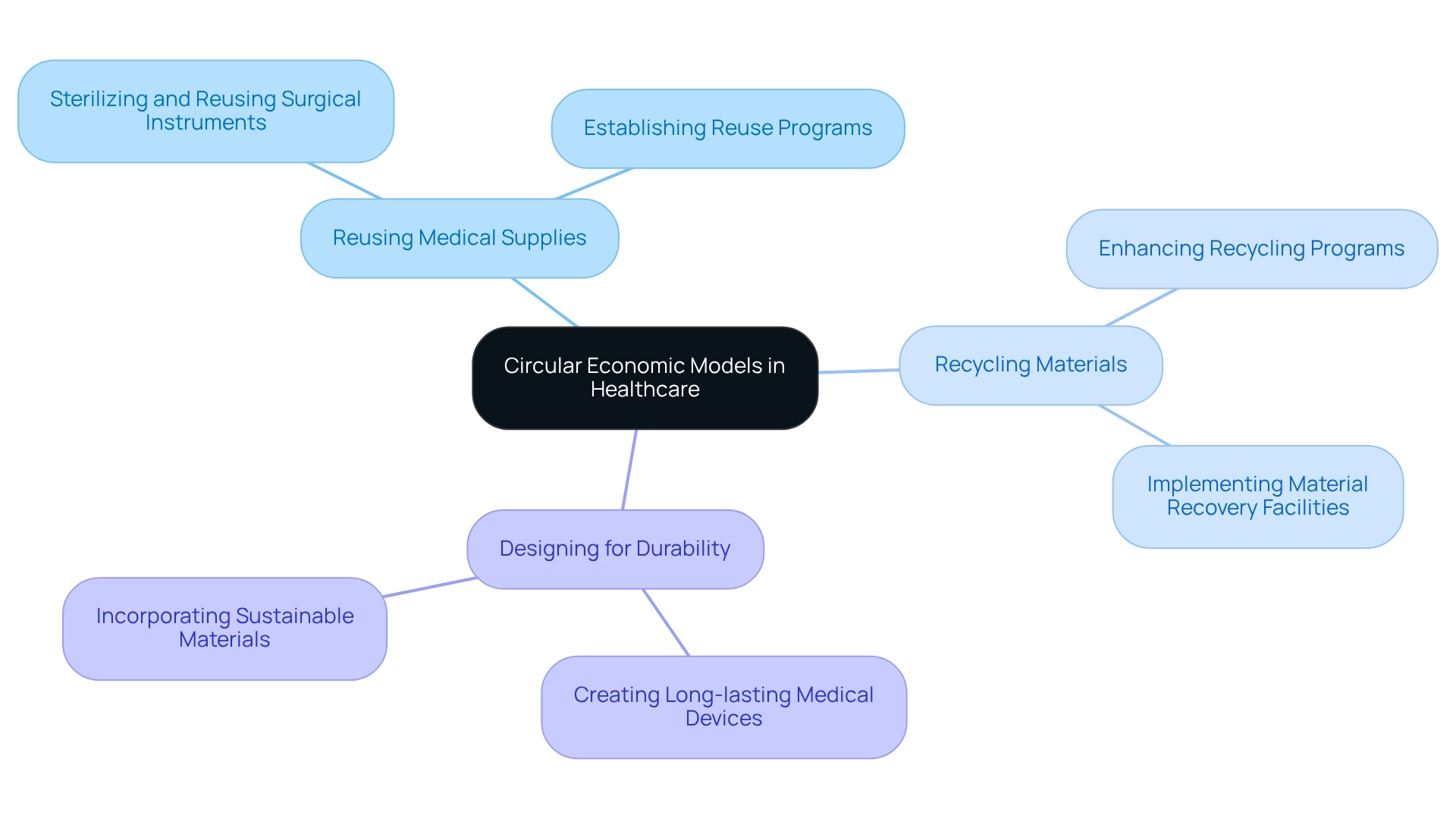
Adopting Circular Economic Models in Healthcare: A Sustainable Approach
Implementing circular economic models in the medical sector necessitates a fundamental transformation in how we utilize and dispose of resources. This approach prioritizes waste reduction through strategies such as:
- Reusing medical supplies
- Recycling materials
- Designing products for durability
For example, we can establish programs to sterilize and reuse surgical instruments, significantly decreasing our reliance on single-use plastics. A notable case study illustrates this: a large hospital network implemented an automated inventory management system, resulting in a 20% reduction in expired medical supplies and a 15% decrease in inventory holding costs. This showcases the effectiveness of such systems in supporting circular economy principles.
By embracing these principles, we not only strengthen our sustainability initiatives but also achieve substantial cost reductions in waste management. Statistics suggest that 92% of studies on medical technologies emphasize the environmental advantages of adopting circular economy practices, reinforcing the necessity for ongoing enhancement in this transition.
While [quick-fix solutions](https://ukwin.org.uk/quotes/Circular Economy) may seem appealing, they often undermine our long-term sustainability goals. As the Waste Framework Directive Experts’ Group notes, excessive reliance on these solutions can detract from more sustainable, long-term strategies. Consequently, a comprehensive strategy that combines recycling and resource efficiency is crucial for the future of our medical services.
To facilitate this transition, we must identify specific areas for continuous improvement, such as enhancing recycling programs and optimizing resource use, ensuring that we are well-positioned to implement circular economy principles effectively.
Overcoming Barriers to Digital Transformation in Healthcare
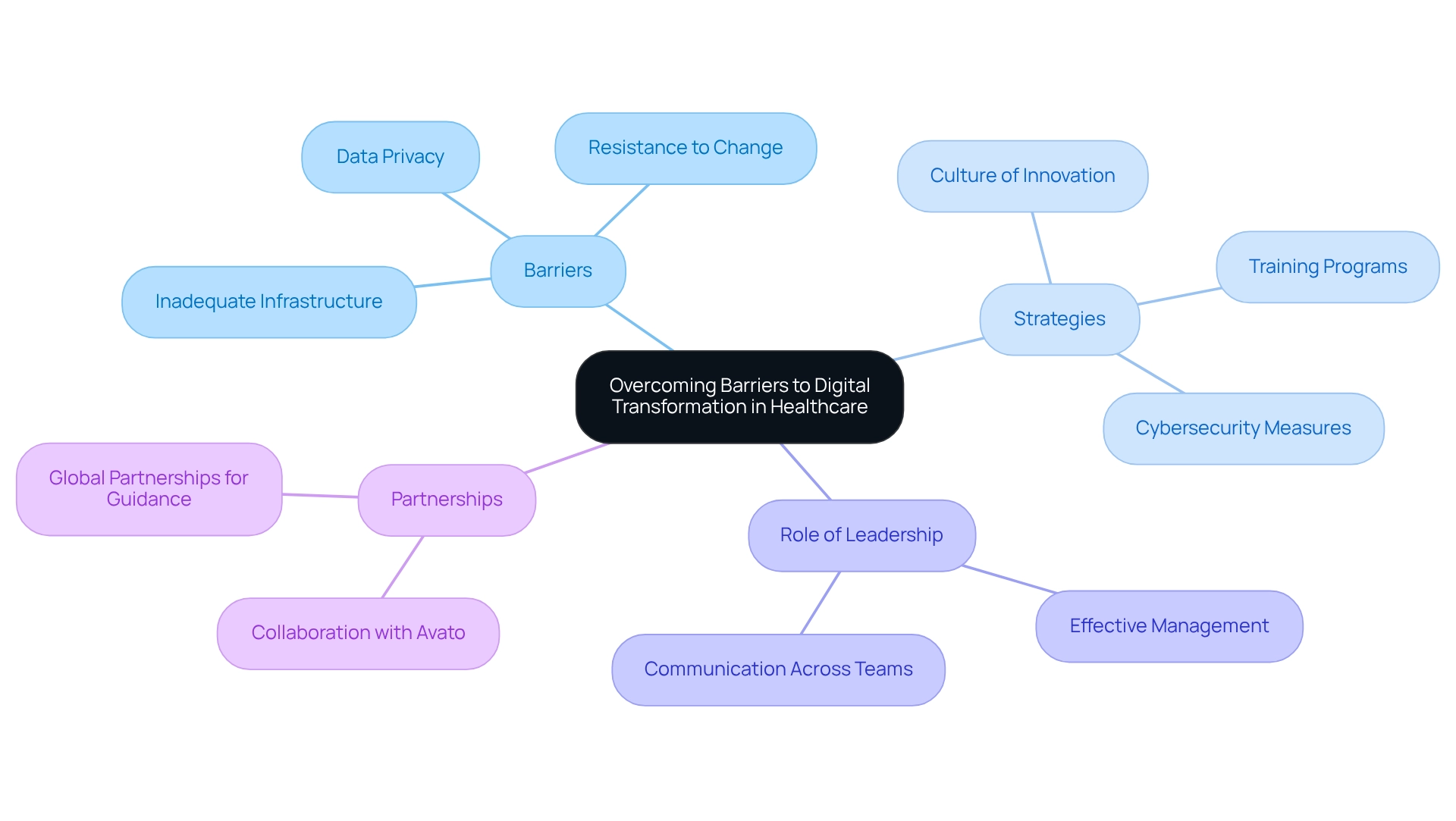
The healthcare digital transformation book highlights that digital transformation in the medical field presents significant barriers, including resistance to change, data privacy concerns, and inadequate infrastructure. A staggering 75% of executives report being unable to fulfill their transformation ambitions, underscoring the urgency for effective strategies. Furthermore, 87% of leaders and analysts believe that technological transformation will disrupt their industry, highlighting the essential need for healthcare organizations to adjust rapidly, a concept explored in the healthcare digital transformation book.
To manage these challenges, we must foster a culture of innovation that promotes adaptability among our employees. Collaborating with Avato can greatly enhance this process; their extensive hybrid integration services—including enterprise architecture, project management, and Red Hat technology—offer the essential tools and support to optimize our technological initiatives.
Training programs centered around new technologies are vital, as data indicates that well-organized training significantly improves staff effectiveness in using electronic tools. Additionally, robust cybersecurity measures are critical in addressing data privacy issues. By ensuring that patient information is secure, we can establish trust and facilitate smoother transitions to electronic solutions. Avato’s global partnerships empower medical providers to leverage expert guidance in implementing these measures effectively.
Leadership plays a crucial role in this process; effective management and communication across teams can accelerate our technological initiatives and cultivate a supportive atmosphere for change. Organizations with strong leadership experience quicker product development cycles and cultural shifts toward technology adoption, ultimately resulting in enhanced outcomes.
Incorporating insights from Maulesh Shukla, an executive manager at Deloitte, it is evident that the future of health and financial transformation in our sector hinges on overcoming these obstacles. By proactively addressing these challenges, as discussed in the healthcare digital transformation book, we can enhance our operational capabilities and prepare for future success in an increasingly technological environment.
To implement these strategies efficiently, we should focus on leadership development and invest in comprehensive training programs that empower our staff to adopt technological tools with confidence, while also considering Avato’s customized solutions to expedite our transformation journey.
Future Trends in Healthcare: The Impact of Digital Transformation
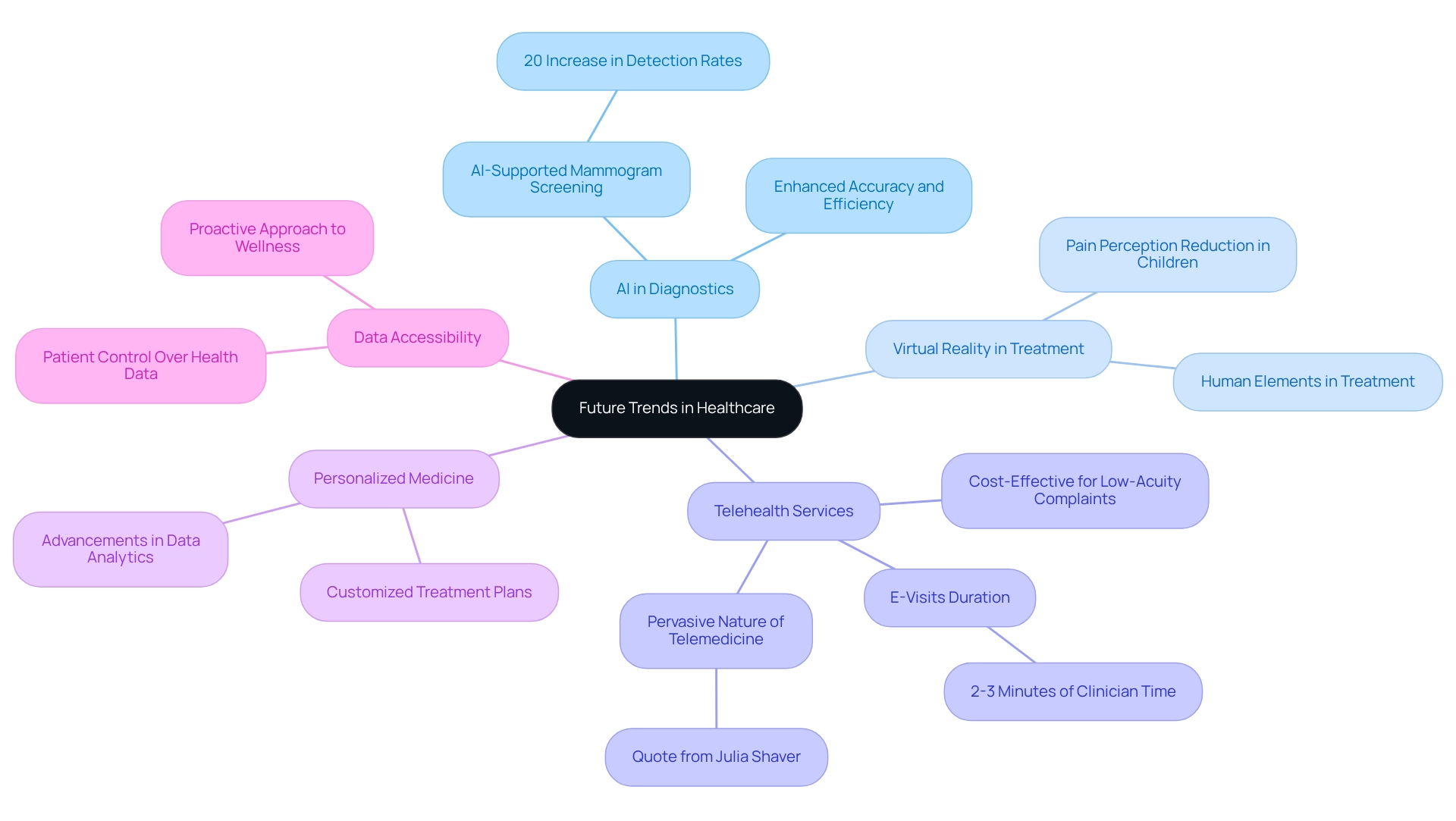
The future of medical services is set for a profound transformation, driven by digital innovation. We are witnessing key trends that are shaping this landscape, including the escalating use of artificial intelligence (AI) for diagnostics and treatment planning. This integration is expected to enhance accuracy and efficiency in healthcare. For instance, AI-supported mammogram screenings have demonstrated a remarkable 20% increase in breast cancer detection rates, showcasing the technology’s potential to improve diagnostic outcomes and exemplifying the broader trend of AI integration in healthcare.
Furthermore, the utilization of AI and virtual reality (VR) is transforming care for individuals by incorporating essential human elements into treatment processes. For example, VR has been shown to considerably lessen pain perception in children during medical procedures, highlighting how digital solutions can significantly enhance user experiences. Moreover, AI-driven avatars can offer tailored assistance and information to individuals, ensuring they receive comprehensive guidance that may not be achievable during brief clinical consultations.
Telehealth services are also on the rise, with e-visits requiring only two to three minutes of clinician time. This makes them a cost-effective solution for managing low-acuity complaints. This shift towards virtual care is likely to persist, as noted by industry experts like Julia Shaver from Kaiser Permanente Northern California, who stated, “It seems clear that telemedicine is likely to remain pervasive in some fashion.” This underscores the enduring role of telemedicine in healthcare delivery.
Moreover, the emergence of personalized medicine, enabled by advancements in data analytics and AI, allows for customized treatment plans that address individual needs. As wearable technology continues to advance, it enables individuals to track their health in real-time, promoting a proactive approach to wellness. The importance of data accessibility cannot be overstated; patients must have control over their health data to explore new treatment options effectively.
We must remain agile, adapting our strategies to harness these emerging technologies effectively. Continuous research is vital to comprehend the long-term effects of telemedicine and AI on medical service delivery. This understanding will be crucial for banking IT managers as they plan their technology investments in the medical sector. As we approach 2025 and beyond, the incorporation of these technological solutions, along with the anticipated substantial expansion of AI in medical services, will be essential in forming a more adaptive and patient-focused system.
Leveraging Data and Digital Innovation for Improved Healthcare Access
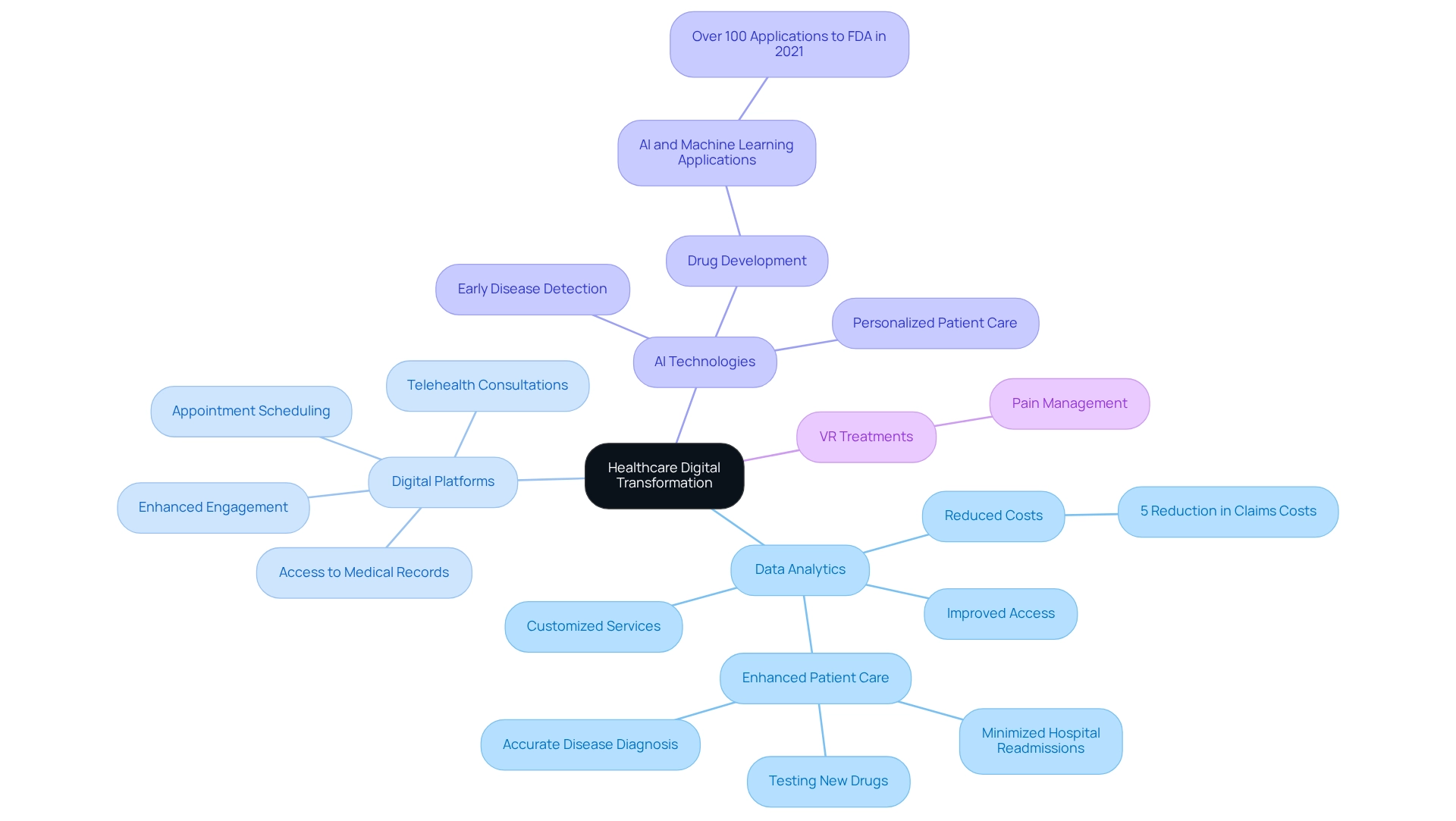
Utilizing data and digital innovation is essential for the concepts discussed in the healthcare digital transformation book, which aims to improve access to medical services. By employing data analytics, we can effectively identify underserved populations and customize services to address their specific needs. The healthcare digital transformation book explains how digital platforms simplify processes like appointment scheduling, telehealth consultations, and access to medical records, significantly enhancing engagement with healthcare services. Furthermore, integrating data from diverse sources provides a comprehensive perspective on health, facilitating more personalized and effective care. The integration of AI and VR technologies further enhances this transformation, as demonstrated by initiatives like virtual reality treatments for pain management and AI-driven interactions that provide detailed health advice, thereby humanizing care, a topic explored in the healthcare digital transformation book.
The healthcare digital transformation book emphasizes that prioritizing data-driven strategies not only enhances access but also leads to improved health outcomes across the board. Statistics indicate that big data analytics in the medical field can reduce claims costs by 5% through tailored insurance plans, showcasing the financial benefits of data utilization. As we observe, the effectiveness of big data analytics in the medical field is discussed in the healthcare digital transformation book, which shows how it assists medical professionals in:
- Testing new drugs
- Diagnosing diseases more accurately
- Reducing hospital readmission rates
- Providing superior care
In 2021, more than 100 drug and biological applications submitted to the FDA employed AI and machine learning, emphasizing the transformative potential of these technologies in early disease detection and individualized care. As medical facilities, including those in Poland, increasingly adopt data-driven approaches, the insights provided in a healthcare digital transformation book highlight the significance of data analytics in enhancing access to medical services. By focusing on data innovation, we can ensure we meet the evolving demands of patients and enhance overall service delivery.
Conclusion
Digital transformation is fundamentally reshaping the healthcare landscape, driving improvements in efficiency, sustainability, and patient care. We recognize that the integration of platforms like Avato’s hybrid system is crucial in bridging the gap between legacy systems and modern applications, ensuring seamless data flow and enhancing interoperability. By enabling healthcare organizations to focus on patient care rather than technical obstacles, we see that these innovations lead to better health outcomes and operational efficiency.
Furthermore, the adoption of sustainable practices within healthcare not only addresses environmental concerns but also enhances operational effectiveness. Strategies such as waste reduction, resource efficiency, and the integration of digital medicine highlight the dual benefits of sustainability and improved patient care. As we embrace technologies like AI and VR, we can further minimize waste and enhance patient engagement, making sustainability an integral part of healthcare’s future.
As healthcare leaders navigate the complexities of digital transformation, we understand that overcoming barriers such as resistance to change and data privacy concerns will be essential. The emphasis on training, robust cybersecurity measures, and leadership development will foster a culture of innovation, enabling organizations to adapt swiftly and effectively.
In conclusion, we believe the future of healthcare is bright with the promise of digital innovation. By leveraging data and technology, healthcare providers can not only enhance access and quality of care but also drive significant improvements in sustainability and operational efficiency. Embracing these trends will position organizations for success in an increasingly digital and patient-centered environment, ultimately ensuring that the focus remains firmly on delivering high-quality care.

